Asthma is a chronic condition characterized by lung airway inflammation that is caused by both genetic and environmental factors.
Asthma is a chronic inflammatory condition affecting the airways of the lungs that is caused by increased airway responsiveness and reversible airway obstruction. This leads to symptoms of chest tightness, wheezing, coughing, and shortness of breath.
When these symptoms occur (usually suddenly), it is known as an asthma attack. Reliever inhalers (normally blue) can be used as effective and quick emergency treatments to combat asthma attacks. However, if emergency inhalers are not available, or medical attention is not immediately sought, asthma attacks can be life-threatening and 3 people die every day in the UK due to untreated asthma attacks.
The worldwide prevalence of asthma has been increasing and continues to rise across the world. More specifically, asthma rates in urban areas are increasing more than in rural areas. Many of the causes of asthma may be attributed to environmental factors such as smoking, air pollution, climate change, but also increasing evidence points towards specific genetic factors that may directly cause asthma in families or predispose individuals to later-onset asthma – especially in combination with environmental factors.
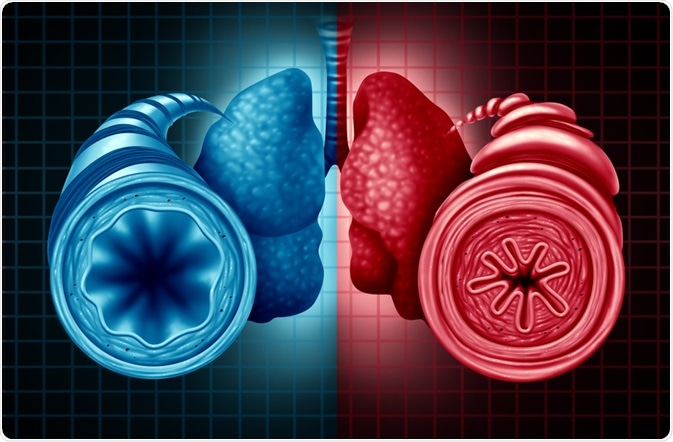 Image Credit: Lightspring/Shutterstock.com
Image Credit: Lightspring/Shutterstock.com
Genetics of asthma
Almost half of all people affected by asthma have a genetic susceptibility – either inherited genetic mutations or single nucleotide polymorphisms (SNPs) which increase the risk of developing asthma especially in combination with certain environmental factors.
For example, people with no family history of asthma have a 5% risk of developing asthma. Having a sibling or a parent with asthma increases this risk to 25%, having both parents with asthma increases this risk to 50%, and having a monozygotic twin increases the risk to 75%. This clearly illustrates a strong genetic basis for asthma risk. The latter also highlights that asthma is not a purely genetic disease and the environment plays an important role in determining asthma risk too (otherwise the risk would be 100% with a monozygotic twin).
Where genes play a strong role as compared to the environment would be primarily in early-onset asthma. Having a family history of asthma usually results in earlier onset disease thus genes may be implicated in the age at onset of disease. Furthermore, the severity of the disease may also be uniform in families e.g., more severe asthmatic parent leading to a severely asthmatic child. Specific genes may increase the risk of allergic asthma (most common) whereas others are involved in non-allergic asthma (rarer but tends to be more severe and usually occurs later in life).
Genes involved in asthma
Most genes implicated in asthma are related to inflammation/modulation of the immune system, or to do with lung physiology. To date, over 100 such genes have been identified – with more being identified each year. These genes include specific cytokines (inflammation/immunity), Toll-like receptors, major histocompatibility complexes (MHC), receptors, cysteine leukotriene metabolic pathway, airway hyperresponsiveness, lung function as well as some other genes.
Specific genes commonly implicated in asthma include:
- ORMDL3 (ORMDL Sphingolipid Biosynthesis Regulator 3) is a gene that is strongly associated with early-onset asthma – leading to high levels of IgE.
- HLA-DQ(A1/B1) is the αβ heterodimer of type MHC class II found on antigen-presenting cells, involved in autoimmune conditions including coeliac disease and diabetes mellitus type 1. Mutations within this gene are involved in late-onset asthma.
- ADAM33 (A Disintegrin and Metalloproteinase 33) is expressed strongly in bronchial smooth muscle cells and lung fibroblasts and is involved in airway hyperresponsiveness and decreased lung function.
- Filaggrin is a gene involved in the maintenance of skin barriers and mutations are typically involved in atopic dermatitis & ichthyosis Vulgaris. Having mutations in this gene usually increases the risk of skin conditions, but also increases the risk of asthma and hay fever on top of those.
- Other commonly implicated genes include (non-exhaustive list):
- IL1RL1 – Interleukin 1 Receptor Like 1 (receptor)
- IL33 – Interleukin-33 (cytokine)
- SMAD3 – SMAD Family Member 3 (intracellular signal transducer protein)
- IL2RB – Interleukin 2 Receptor Subunit B (receptor subunit)
- SPINK5 – Serine Peptidase Inhibitor Kazal Type 5 (multidomain serine protease inhibitor)
- VDR – Vitamin D Receptor (receptor)
- DPP10 – Dipeptidyl Peptidase Like 10 (membrane protein)
- PHF11 – Ph.D. Finger Protein 11 (Ph.D. type zinc finger)
- HLA-G – Human Leukocyte Antigen G (MHC)
- IL13 – Interleukin-13 (cytokine)
- GPR15 – G Protein-Coupled Receptor 15 (receptor)
- TLR2/4/6/9/10 – Toll-Like Receptors 2, 4, 6, 9 & 10 (receptors)
Many of these genes are involved in inflammation, immunity, and lung function. Mutations or polymorphisms to any of these genes compromise their normal function thus leading to dysregulated immune/inflammatory responses (i.e., exaggerated response), or remodeling of the airways decreasing lung function, or increasing hyperresponsiveness.
Collectively they contribute either to causing earlier-onset asthma, or predisposing adults to developing asthma later in life in combination with certain environmental factors (such as smoking, air pollution, dust mites, or pollen) or combination with other conditions such as dermatitis.
In summary, asthma is a complex multifactorial condition that has many causes – both environmental and genetic. Having a family history of asthma increases the risk of asthma thus suggesting a strong genetic basis. Certain genes may only predispose individuals to asthma (later-onset/environmentally triggered), however, other genes may be directly causative of asthma – particularly early-onset or that which is more severe (typically running in families). Knowing what genes cause asthma or increase the risk of asthma is important in the development of novel therapies and treatments.
References
- Huo & Zhang, 2018. Genetic Mechanisms of Asthma and the Implications for Drug Repositioning. Genes (Basel). 9(5):237. https://pubmed.ncbi.nlm.nih.gov/29751569/
- Thomsen, 2015. Genetics of asthma: an introduction for the clinician. Eur Clin Respir J. 16;2. https://pubmed.ncbi.nlm.nih.gov/26557257/
- Jindal, 2015. Genetic basis of asthma. Indian J Med Res. 142(6):640-3. https://pubmed.ncbi.nlm.nih.gov/26831411/
Further Reading
- All Asthma Content
- Asthma
- Childhood Asthma
- Signs of Asthma Attack
- Asthma Symptoms
Last Updated: May 4, 2021

Written by
Dr. Osman Shabir
Osman is a Postdoctoral Research Associate at the University of Sheffield studying the impact of cardiovascular disease (atherosclerosis) on neurovascular function in vascular dementia and Alzheimer's disease using pre-clinical models and neuroimaging techniques. He is based in the Department of Infection, Immunity & Cardiovascular Disease in the Faculty of Medicine at Sheffield.
Source: Read Full Article