It is known that the tumor microenvironment plays an important role in the progression of cancer. But could estrogen present in this microenvironment facilitate the growth of liver metastases in women affected by colon, pancreatic and lung cancers? This is what a team of researchers from the Research Institute of the McGill University Health Centre (RI-MUHC) suggests, in a study that shows for the first time that the liver immune microenvironment reacts to metastatic cells differently in male and in female mice and that, indeed, the main female hormone estrogen can indirectly contribute to the growth of metastases. Their findings, recently published in Nature Communications, provide a rationale for further exploration of the role of sex hormones in female cancer patients and the potential benefits of anti-estrogen drugs such as tamoxifen in the treatment of hormone-independent cancers that metastasize to the liver.
“What prompted us to begin this investigation was our finding that the immune microenvironments of liver metastases in male and female mice are regulated differently,” says Dr. Pnina Brodt, senior scientist in the cancer research program at the RI-MUHC and lead author of the study. “We were also aware of reports based on recent immunotherapy clinical trials that female patients do not respond to immunotherapy as well as male patients and that overall, patients with liver metastases respond more poorly to such treatments than patients without liver metastases.”
“We therefore wanted to identify factors unique to male and female responses to liver metastatic disease that could explain these findings and could eventually lead to improved immunotherapy outcomes for patients,” adds Dr. Brodt.
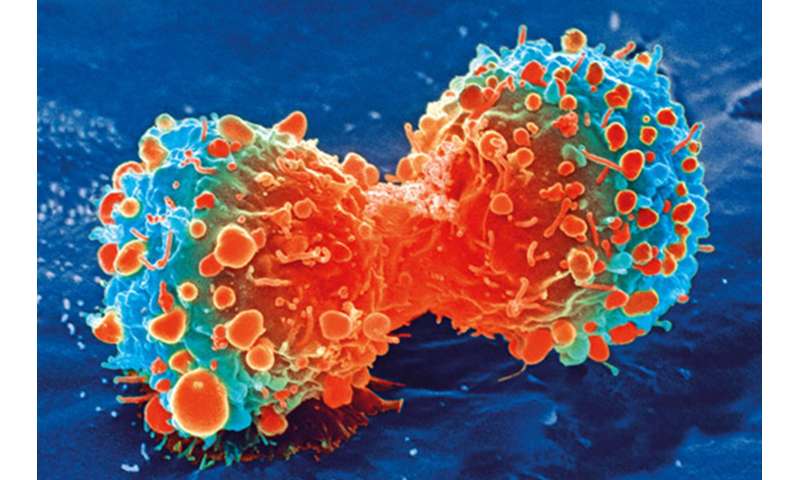
Dr. Brodt and her team looked at the interaction between metastatic cells entering the liver and the unique microenvironment of this organ, in mouse models of colon, pancreatic and lung carcinoma, malignant diseases that do not have a clear sex bias and are not depended on sex hormones for growth.
By increasing and decreasing the levels of estrogen in their mouse models, the team discovered that estrogen plays a role in the expansion of liver metastases—a major cause of cancer-associated death. Specifically, they found that this hormone regulates the accumulation in the liver of bone marrow-derived innate immune cells such as the myeloid-derived suppressor cells (or MDSC) and immunosuppressive macrophages.
Cancer cell killers can become friends of the enemy
When metastatic cells enter the liver, innate immune cells are recruited, some from the bone marrow. These cells have the ability to kill cancer cells, but once in the tumor environment, they can also acquire immunosuppressive and tumor promoting functions.
MDSCs, for instance, do not directly affect cancer cell growth, but can do so by changing the microenvironment around the tumor in the liver.
“MDSCs can impede the activity of T lymphocytes, whose role is to kill the cancer cells. In this way, they act to promote—rather than curtail—the growth of metastases,” explains Dr. Brodt, who is also Professor in the Departments of Surgery, Oncology and Medicine at McGill University.
The team observed that estrogen induces an immune tolerant environment that helps the tumor cells grow, and that the removal of estrogen reduces the accumulation and activity of MDSCs that, in some way, become “friends” of the enemy.
“The realization that cancer is a community of cells, not just the cancer cells, but also the cells that surround it has become an important part of how the scientific community now views cancer and how it should be treated,” says Dr. Brodt.
Toward gender-specific cancer treatment?
In this era of personalized cancer management and with the worldwide effort to develop drugs that target the tumor microenvironment, awareness of the fact that male and female patients may respond differently to such treatments is very important.
“This should now be taken into account to design better, more gender-specific treatment strategies, especially when we know that colorectal cancer incidence, for instance, is increasing in the younger population,” says Dr. Brodt.
There are several approved anti-estrogen drugs currently in routine clinical use. However, their use is restricted to patients with hormone-sensitive cancers such as breast cancer.
Source: Read Full Article