Damage to the facial nerve, cranial nerve VII, results in facial paralysis, which is commonly referred to as facial palsy. The seventh cranial nerve is responsible for innervating the facial muscles and has its origin in the pons.
It works its way via a long winding path through the skull, before exiting through the foramen of the stylomastoid on the temporal bone. The consequence of its paralysis is a loss of control of the facial muscles, which appear to droop. Sometimes only one side of the face is affected and in other instances both halves may be affected. 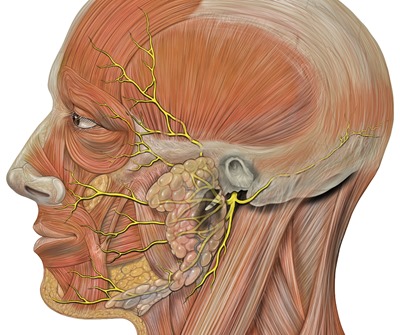
Photo credit to Patrick J. Lynch, medical illustrator / commons.wikimedia.org
Causes
Facial palsy may be congenital (i.e. present at birth), caused by trauma during birth, or be the result of developmental defects that damage or obliterate the facial nerve in utero. The conditions that may lead to acquired facial paralysis are many. In many cases, the cause of facial palsy is idiopathic (i.e. unknown) and it is then called Bell’s palsy.
Despite being classified as idiopathic there is evidence that suggests this condition may possibly be associated with a herpes simplex virus infection. Bell’s palsy is responsible for approximately 6 in every 10 cases of facial paralysis with an acute onset, and is estimated to affect up to 40 per every 100,000 people every year.
Other causes of facial palsy include tumors, stroke and trauma, especially to the temporal bone. Some rarer causes of facial palsy include multiple sclerosis, otitis media and neurosarcoidosis. A tumor that compresses the facial nerve anywhere along its path through the skull may lead to facial paralysis.
More common than neoplastic causes is iatrogenic facial nerve palsy, where there is inadvertent damage to the facial nerve during tumor removal. A classic example would be nerve damage occurring during the removal of an acoustic neuroma, a benign tumor on the nerve responsible for hearing.
Ramsay Hunt syndrome, which is caused by infection with herpes zoster, presents with herpetiform vesicular lesions, dysfunction of the vestibulocochlear apparatus, and facial paralysis. In contrast to Bell’s palsy, Ramsay Hunt syndrome is more painful, has a lower rate of recovery, and a significantly higher risk of hearing loss. Another infectious cause of facial paralysis is Lyme disease that follows bites by ticks infected with Borrelia burgdorferi. Approximately 10% of patients with Lyme disease develop facial nerve paralysis and a quarter of these may have bilateral facial paralysis.
Management
Pharmacotherapy and surgical operations may be necessary for managing facial palsy, depending on the etiology. Corticosteroids together with antiviral agents administered within a period of 72 hours are used to treat Ramsay Hunt syndrome and Bell’s palsy. Patients with tumors as the cause of their facial paralysis will need to have their tumors surgically resected if possible.
Advanced surgical procedures for patients that have lost the function of their facial nerve, include facial re-animation, with nerve grafts, or muscle transposition and plastic surgery, which is done to improve facial symmetry at rest. The latter is known as a static surgery.
Physiotherapy may also be necessary depending on the extent and duration of the facial paralysis. Some common techniques employed for physiotherapy include neuromuscular retraining, trophic electrical stimulation, electromyography biofeedback and proprioceptive neuromuscular facilitation.
References:
- http://www.facialpalsy.org.uk/
- http://bellspalsy.org.uk/links.html
- http://www.nhs.uk/Conditions/Bells-palsy/Pages/Introduction.aspx
- http://jamanetwork.com/journals/jama/fullarticle/184482
- http://www.cmft.nhs.uk/royal-eye/our-services/facial-function-clinic.aspx
Last Updated: Jun 16, 2019

Written by
Dr. Damien Jonas Wilson
Dr. Damien Jonas Wilson is a medical doctor from St. Martin in the Carribean. He was awarded his Medical Degree (MD) from the University of Zagreb Teaching Hospital. His training in general medicine and surgery compliments his degree in biomolecular engineering (BASc.Eng.) from Utrecht, the Netherlands. During this degree, he completed a dissertation in the field of oncology at the Harvard Medical School/ Massachusetts General Hospital. Dr. Wilson currently works in the UK as a medical practitioner.
Source: Read Full Article