 By Keynote ContributorDr. Xiangjian ZhengHead of Lab of Cardiovascular Signaling,
By Keynote ContributorDr. Xiangjian ZhengHead of Lab of Cardiovascular Signaling,Centenary Institute, Sydney Medical School
Written by Dr Zheng, PhD
Cerebral cavernous malformation (CCM), also knows a cavernous hemangioma, cavernous angioma or cavernoma, is a brain blood vessel malformation characterized by irregularly clustered small thin-walled blood vessels.
These abnormal vessel clusters can occur in any part of brain and spinal card, although mostly found in white matter. They can be progressive, but are not cancerous.
These abnormal vessels are filled with slow-moving or stagnant blood and are fragile. Bleeding from the lesions or displacement of neuronal tissue by the enlarged lesions are the underlying causes of clinical symptoms.

Prevalence
CCM has been estimated to affect up to 0.5% in human population. About 80% of cases occur in a sporadic form (without family histology), and 20% of cases occur in a hereditary (familial) form.
The sporadic cases often only have a single lesion, while the familial cases often present with multiple lesions. The lesion size in both form of CCM can vary from a few millimeters to a few centimeters.
About 60% of familial cases are symptomatic, most of them manifest symptoms in 20-30 year of age. The percentage of symptomatic cases in sporadic form is not easily assessable.
In general, CCM can develop at any age, no preference for male or female, or a particular ethnic population. Among all the diagnosed cases, about 25% are children.
Symptoms and diagnosis
The symptoms of CCM disease are variable neurological manifestations including: seizure, non-specific headaches, progressive or transient focal neurologic deficits (such as cranial nerve deficits, sensory deficits, difficulty with vision or speech, weakness in arms or legs, dizziness, nausea and vomiting, problem with balance, muscle coordination or memory).
CCM are diagnosed according to these symptoms and MRI scans. For patients with atypical MRI, genetic test of CCM genes is necessary to ascertain diagnosis.
For diagnosed patients with multiple lesions, family history of CCM disease characteristics, or very young onset age, genetic tests for patients and related family members are recommended.
Causes
Genetic studies with familial cases of CCM have identified mutations is CCM1, CCM2 or CCM3 causes CCM lesions. Mutations in these three genes accounts for about 90% of all familial cases, the cause of the rest 10% arises from other unknown cause.
Somatic mutations in these three genes have also been identified in sporadic cases of CCM. Among these three genes, mutations in CCM1 and CCM2 gene are more common, together account for 70-80% of familial cases, whereas mutations in CCM3 gene accounts for about 15% of familial cases.
But Mutations in CCM3 gene cause greater lesion burden and higher risk and early onset of hemorrhage, usually within 10 years old in age. Patients with CCM3 mutations more likely devastated by lesion burden and repeated hemorrhages.
Treatment
Currently there is not drug available to treat CCM. The only treatment option is surgical removal. The decision for operation need to be made based on surgery risk of approaching the location of lesions and risk of life-treating hemorrhage or neuronal tissue displacement, especially for the cases with CCM lesion sin brain stem.
After diagnosed with CCM, generally annual MRI is recommended for patients assess the stability of diagnosed lesion and any new asymptomatic lesion. Treatment for seizure and headache are provided if they are the symptoms. Surgical operation is assessed according the risks for patients with recent severe hemorrhage, or severe disabling seizures or neurologic deficits.
Research to understand the disease
Since the identification of three disease genes, scientists around the world are working hard to understand what the function of these genes is in normal life and how damages of these genes cause disease.
Using animal models and cultured human cells, scientists have found proteins produced from three genes working together to maintain the tight interaction between blood vessel cells. These proteins are essential for the formation of lumen in blood vessel.
Animals with complete loss of these genes before birth cannot form functional blood vessel systems to support blood flow. Using genetic tools to delete the disease genes, mice will form CCM lesions mimicking those in humans.
With this mimicking animal model, scientists have found a few other proteins that are critical for CCM lesion formation, which are being considered as potential drug targets.
Using the most advanced tools, Scientists at the Centenary Institute and University of Pennsylvania have recently found 3 additional proteins that mediate the function of damaged CCM proteins. Genetically deleting any one of them is sufficient to prevent the development of CCM disease.
Therefore, blocking the production or activity any of these proteins will potentially treat CCM disease. The Zheng Lab at Centenar
y Institute is currently collaborating with medical chemist at Monash Institute of Pharmaceutical Sciences to search for a drug to block these abnormally increased proteins.
Currently two drugs, both targeting the activity of a particular protein, called ROCK, are in development in two small biotech companies in USA. Both are still in the early testing phase in cell culture and animal studies, so it is still not clear whether they will be effective enough to reach the phase of clinical trial.
About Dr Zheng
Dr. Xiangjian Zheng obtained his PhD in Molecular Medicine from Medical College of Georgia. He received postdoctoral training from Department of Pharmacology at Vanderbilt University and Cardiovascular Institute at University of Pennsylvania School of Medicine.
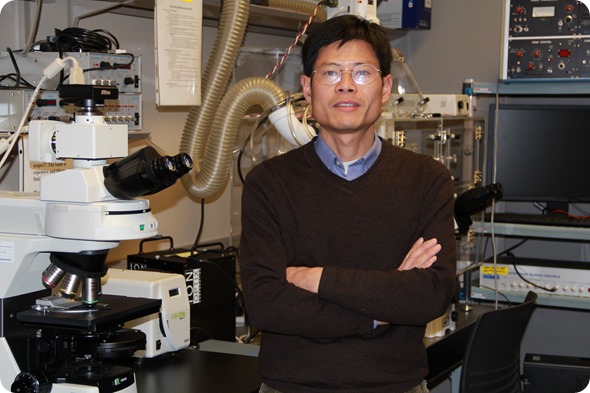
He joined the faculty of Centenary Institute to lead the Lab of Cardiovascular Signaling in 2014. He is also a member of Faculty of Medicine at Sydney University. Dr. Zheng started to work on CCM disease in 2006.
Since then he has made major contributions to CCM research by generating advanced animal models, developing new CCM imaging method in animal models and identifying a series of new molecular players and their integrative functions in CCM pathogenesis.
His work has been published in top biomedical research journals including Nature, Nature Medicine, Journal of Clinical Investigation, and Developmental Cell. His current research is expanding from basic research to translational studies in searching for drug candidates to treat CCM disease.
Disclaimer: This article has not been subjected to peer review and is presented as the personal views of a qualified expert in the subject in accordance with the general terms and condition of use of the News-Medical.Net website.
Last Updated: Jun 28, 2019
Source: Read Full Article