Menopause is defined as the cessation of a woman’s menstrual periods for more than 12 consecutive months and is due to the non-functioning of her ovaries. It may occur spontaneously, the average age of onset being 51 years. However, it may also occur following surgery or cancer treatment.
Surgical menopause refers to the onset of menopause after the surgical removal of both ovaries. It is followed by the immediate end of menstruation and a drastic drop in sex hormones. Menopausal symptoms set in almost at once. Surgical menopause also occurs in a woman who undergoes a total or radical hysterectomy, which implies the removal of both ovaries as well as the whole of the uterus.
Surgery to remove the ovaries is not always necessary or indicated in women who are having a hysterectomy. Some recommendations include:
- Ovary removal if there is a significant risk of disease, including ovarian cancer
- Prophylactic removal if your family has a history of ovarian or breast cancer
Spontaneous menopause is likely to occur within five years of having a hysterectomy, even though the ovaries are spared. This is because of disturbances in the ovarian blood supply, which leads to a gradual decline in ovarian function.
Surgical menopause is differentiated from spontaneous menopause by the fact that even after monthly cycles stop in the latter, the ovaries continue to generate small amounts of estrogen and testosterone, which contribute to sexual desire or pleasure. Surgical menopause thus leads to greater loss of sexual function and more distress in this area.
Symptoms
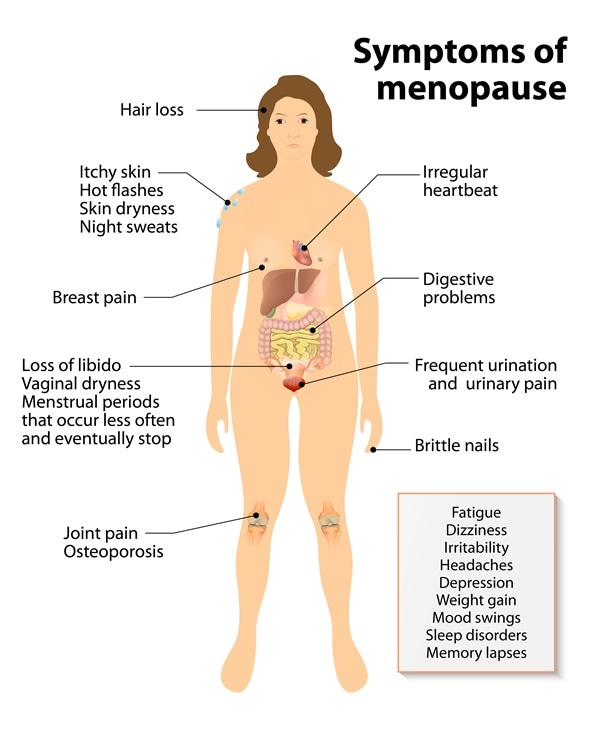
Symptoms of menopause include:
- Vasomotor symptoms such as hot flushes and sweating
- Decreased sexual desire
- Fatigue
- Insomnia
- Mood shifts
- Depression
- Vaginal dryness
- Cognitive decline
Management of surgical menopause
If a woman has a total hysterectomy before the age of 40, she will experience symptoms of premature or early menopause. Mortality and morbidity is higher in women who undergo early menopause, because of the increased risk of ischemic heart disease, osteoporosis and cognitive decline.
General measures to ease the menopausal transition include:
- Ensuring a healthy diet with
- 7 daily servings of fruits and vegetables
- 6 daily servings of whole grains or their products
- 3 daily servings of milk or milk substitutes
- 2 daily servings of meat or meat alternatives
- Cutting down on sodium and simple sugars
- Avoiding saturated and trans fats
- Supplementing vitamin D as well as calcium
- Managing your weight
- Regular physical exercise
- Avoiding or quitting smoking
- Avoiding or quitting alcohol and hot drinks, in case of vasomotor symptoms
Hormone replacement therapy
If the symptoms of surgical menopause are very severe, or the patient desires symptom alleviation, it is wise to discuss the possibility of hormone replacement therapy (HRT). This consists of estrogen and progesterone in combination, for women who still have their uterus, or estrogen alone, after a total hysterectomy.
Contraindications to this mode of treatment would include a personal or family history of breast cancer, or some types of liver disease. Once started, HRT is usually continued till the age of 51. Recent recommendations are that HRT be continued with appropriate dosage adjustments, on a case-by-case basis, till no longer required. The woman may require additional therapies to mitigate associated health conditions such as osteoporosis.
Treatment of dyspareunia or incontinence
Vaginal estrogen therapy helps to improve the condition of the mucosa, in cases of dyspareunia or incontinence. Other measures to strengthen the pelvic floor muscles, including pelvic exercises, weighted vaginal cones and pessaries, are also useful.
Psychological issues following surgical menopause
Surgical menopause may trigger both relief and stress. Women who have struggled with bleeding problems or pain related to menstruation may welcome the cessation of their symptoms after oophorectomy (surgical removal of one or both ovaries). On the other hand, those who already have psychological disturbances may find that menopause pushes them over the edge into depression, anxiety, hostility or mental instability. It may also cause a fall in sexual desire. The abrupt loss of both estrogen and androgens is thought to be partly responsible for this psychological change.
Effects on immune function
Surgical menopause may bring about diverse effects on the immune function resulting in impaired immunity, caused by estrogen deficiency. Estrogen replacement therapy can bring about an improvement in immune status.
Cognitive decline
Estrogen has a neuroprotective effect, with a rapid and precipitous drop in estrogen levels (below 50 percent) being linked to greater cognitive decline and dementia, including Alzheimer’s disease. Removal of one or both ovaries before spontaneous menopause increases the risk of these conditions in an age-dependent manner, with younger women being at greater risk.
Alternative medicine has much to offer in alleviating the effects of surgical menopause, but most of the products in this field are empirically prescribed, not being backed by valid clinical research. However, a woman in good physical, mental and emotional health who is ready to take charge of her health can usually find a way to get through the distressing symptoms of menopause using some of the methods above.
References
- http://womenshealth.gov/menopause/early-premature-menopause/
- http://www.nhs.uk/Conditions/Hysterectomy/Pages/Considerations.aspx
- http://www.ncbi.nlm.nih.gov/pubmed/11304879
- http://www.ncbi.nlm.nih.gov/pubmed/15284002
- http://www.ncbi.nlm.nih.gov/pubmed/11893842
- http://www.ncbi.nlm.nih.gov/pubmed/17476145
- http://sogc.org/wp-content/uploads/2014/09/gui311CPG1409Eabstract.pdf
- http://www.neurology.org/content/69/11/1074.short
Further Reading
- All Menopause Content
- What is Menopause?
- Causes of Menopause
- What Should I Eat During Menopause?
- Menopause Symptoms
Last Updated: Feb 27, 2019

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article