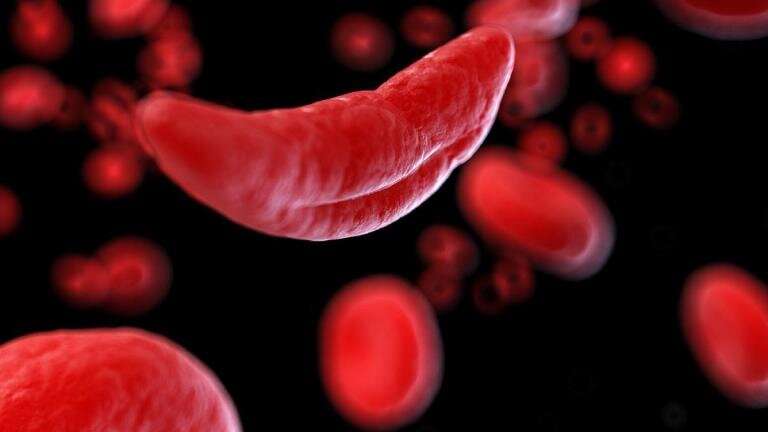
New research led by Nansi Boghossian, associate professor of epidemiology, has investigated the relationship between sickle cell disease and severe maternal morbidity (i.e., adverse outcomes such as heart failure, blood transfusions, and hysterectomy after delivery). In research published in JAMA Pediatrics, strattera spelling the authors found that sickle cell disease was an important contributor to racial disparities in adverse maternal health outcomes.
“Severe maternal morbidity is a major public health crisis and has been increasing in the United States,” Boghossian says. “Black individuals bear the disproportionate burden of these unintended effects, which can have both short- and long-term consequences.”
Despite significant medical advancements, the overall rate of severe maternal morbidity has increased dramatically over the years, according to the Centers for Disease Control and Prevention. More than 50,000 individuals are affected each year, and Black individuals are at least 1.5 times more likely to experience these complications than White individuals.
To explain these disparities, previous research has pointed to a higher prevalence of clinical risk factors (e.g., preeclampsia, chronic hypertension, diabetes) among Black individuals. However, these studies overlooked the role of sickle cell disease in the differences.
Boghossian and her team examined hospital records from more than 8.5 million deliveries across five states between 2008 and 2020. They found that sickle cell disease accounted for 8.9 percent of the Black-White disparity in severe maternal morbidity and 14.3 percent of the disparities in severe maternal morbidity that excluded blood transfusions (a common secondary way of looking at morbidities that are truly severe due to lack of information on the number of transfused units).
Because most sickle cell disease cases occur among Black individuals, the researchers also examined risk ratios within this population. Their analyses revealed a nearly four-fold increased adjusted risk ratio of severe maternal morbidity. They also found that 11 percent of Blacks with sickle cell disease experienced more than one type of severe maternal morbidity, with 14 of every 10,000 of these individuals losing their lives during delivery.
“We know that many factors—including clinical factors such as hypertension, quality of care, racism, sociodemographic variables and others—contribute to racial disparities in severe maternal morbidity, and now we have evidence that sickle cell disease plays an important role as well,” Boghossian says.
“Regardless of whether this condition impacts severe maternal morbidity directly or indirectly through other pregnancy complications, it is a hereditary disease that is present long before pregnancy. Preconception care and management, including screening and counseling by a multidisciplinary team of health care professionals is critical for improved pregnancy outcomes for patients with sickle cell disease.”
More information:
Nansi S. Boghossian et al, Association of Sickle Cell Disease With Racial Disparities and Severe Maternal Morbidities in Black Individuals, JAMA Pediatrics (2023). DOI: 10.1001/jamapediatrics.2023.1580
Journal information:
JAMA Pediatrics
Source: Read Full Article