Researchers at the Thoracic Surgery research group, the Department of Molecular Medicine and Surgery, have performed a nation-wide study of patients who underwent bioprosthetic aortic valve replacement in Sweden between 2003 and 2018. The study is published in the Journal of the American College of Cardiology, kenalog injection j code JACC, and shows that it is less dangerous than previously believed to receive a small bioprosthetic aortic valve in relation to the patient’s size.
During surgical aortic valve replacement, the patient receives a valve prosthesis that matches the size of the aortic root. Sometimes, that size is too small in relation to the patient’s body size. This puts strain on the heart to pump enough blood that the body needs through a narrow valve. The level of “narrowness” is measured as Prosthesis Patient Mismatch, PPM.
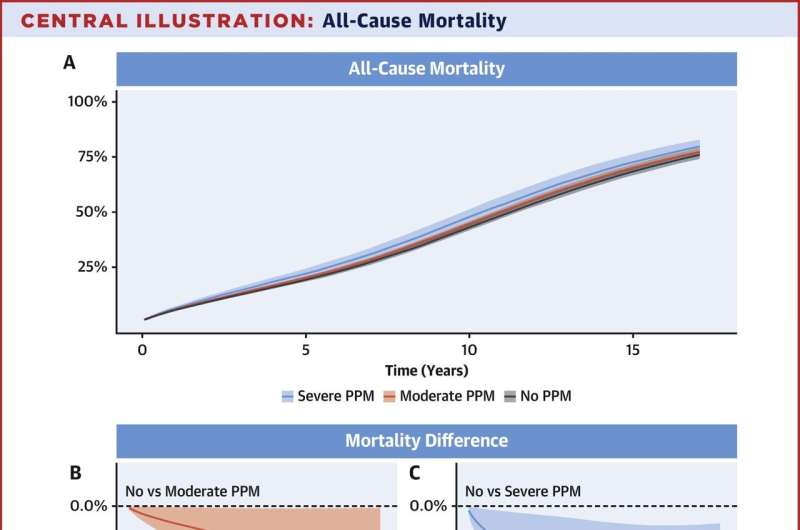
“Prior studies have shown that both moderate and severe PPM decreases survival and increases the risk for heart failure. In our study, we can confirm that severe PPM decreases survival and increases the risk for heart failure, while moderate PPM has a very limited effect on survival and no effect on the risk for heart failure,” says Michael Dismorr, postdoctoral researcher at the Department of Molecular Medicine and Surgery and first author of the study.
The study included all patients who underwent bioprosthetic aortic valve replacement in Sweden between 2003 and 2018. Patients were identified from the Swedish cardiac surgery register, part of the SWEDEHEART register. The database was enriched with data from other national health data registers. By using the statistical method regression standardization we were able to estimate the risk for the outcomes death, heart failure and reintervention in absolute terms between the groups no, moderate and severe PPM.
The study shows that the estimated risk difference between no and moderate PPM for death after 10 years of follow-up was -1.7% (-3.3% to -0.1%) compared to -4.6% (-8.5% to -0.7%) for severe PPM.
The risk difference for heart failure after 10 years of follow-up was -1.1% (-2.5% to 0.2%) between patients with no and moderate PPM.
“A risk difference of a single percent after 10 years of follow-up cannot be said to be of clinical significance, even if it is statistically so. However, it is important to note that these are hard clinical outcomes. We did not have access to “soft” outcomes such as quality of life, which might be decreased in patients with moderate PPM, and in that case of course of great importance to those patients,” says Michael Dismorr.
“Now we want to study the effect of PPM in patients who underwent transcatheter aortic valve replacement, a so called TAVR procedure. This is important knowledge when deciding which patients will benefit the most from a surgical replacement, and which patients will benefit the most from a transcatheter replacement,” says Michael Dismorr.
More information:
Michael Dismorr et al, Effect of Prosthesis-Patient Mismatch on Long-Term Clinical Outcomes After Bioprosthetic Aortic Valve Replacement, Journal of the American College of Cardiology (2023). DOI: 10.1016/j.jacc.2022.12.023
Journal information:
Journal of the American College of Cardiology
Source: Read Full Article