Having a child is both an exciting as well as stressful time in life. However, with the onset of the coronavirus disease 2019 (COVID-19) pandemic, women have struggled with difficulties in accessing care and, as a result, the inability to have in-person talks with their healthcare providers.
Pregnant women, aleve $3 coupon in particular, often fear contracting the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and being alone due to social distancing regulations during their visits to the hospital, especially in the intrapartum period.
A new study published on the preprint server medRxiv* discusses the effects of stress during pregnancy in the pandemic on the developing brain of the infant. The results of the current study indicate the need for urgent policy changes to better care for pregnant women, thus improving both their mental health and the formation of fetal neural connections.
 Study: Prenatal Maternal Distress During The COVID-19 Pandemic and Its Effects on The Infant Brain. Image Credit: Connect world / Shutterstock.com
Study: Prenatal Maternal Distress During The COVID-19 Pandemic and Its Effects on The Infant Brain. Image Credit: Connect world / Shutterstock.com
Background
The effects of the pandemic have been wide-ranging, from hospitalizations with severe illness or death, to closures of a wide range of public institutions from schools and playgrounds to businesses. Travel restrictions and limits on social interactions have also significantly impacted the economy.
Among the many consequences of the current pandemic is prenatal distress, which the researchers define as “elevated symptoms of anxiety and/or depression.” Prenatal distress is associated with undesirable effects on both the pregnant woman and the developing fetus, such as preterm birth, as well as increased risks of behavioral and mental health problems in the offspring.
These effects are likely to arise from aberrant development within the limbic system, which leads to the altered formation of behavior patterns. It is especially true that this affects the structure of brain nuclei like the amygdala, white matter, and connections between the amygdala and the prefrontal regions.
The white matter is composed of neuronal fibers that allow for the billions of cross-connections that underlie the brain’s enormous and complex activity. The pathways between the amygdala and prefrontal regions are responsible for the child’s behavioral response to maternal stress, such as hyperactivity and aggression.
Thus, the disruption of brain structure mediates the abnormal development of child behavior when born to mothers with prenatal distress.
A striking aspect of the pandemic, with regard to pregnant mothers, has been the loss of healthcare and social support for expectant and new mothers. The rates of mental distress during pregnancy have increased by a factor of more than three since the pandemic began. This is a concern, given the findings of earlier studies that demonstrate how prenatal distress affects brain development and behavior over the long term.
These indications give rise to fears about the upcoming generation of pandemic-born children, especially the potential for issues with their cognitive development in early infancy and childhood.
Another important bit of knowledge relates to the protective effect of social support on the neurological and psychological changes accompanying prenatal distress. The current study took this further, examining the potential for social support to prevent the disruption of infant brain development as a result of prenatal distress.
The aim of the current study was to determine if this was a modifiable risk factor. Ultimately, the researchers hope that their findings will help shape health policies to target children at high risk and produce rapid changes in their environment.
Study findings
The current study used data from the Pregnancy during the COVID-19 Pandemic (PdP) study that covered most of Canada. All participants were less than 35 weeks pregnant. Their mental health was assessed using the Edinburgh Depression Scale (EPDS) for depression, the Patient Reported Outcomes Measurement Information System (PROMIS) Anxiety for anxiety, and the Social Support Effectiveness Questionnaire (SSEQ) to evaluate the quantity and quality of social support the pregnant woman was obtaining.
The study showed a mean EPDS score above 10, with a third of the participants being clinically depressed with scores of more than 12. The mean PROMIS score was also high, and almost half the participants had clinical anxiety symptoms. The SSEQ scale, meanwhile, touched 50 on average.
These results demonstrated higher prenatal maternal distress after the pandemic began, even after adjusting for ethnic origin and race. The higher the SSEQ, the less the chances of significant prenatal distress.
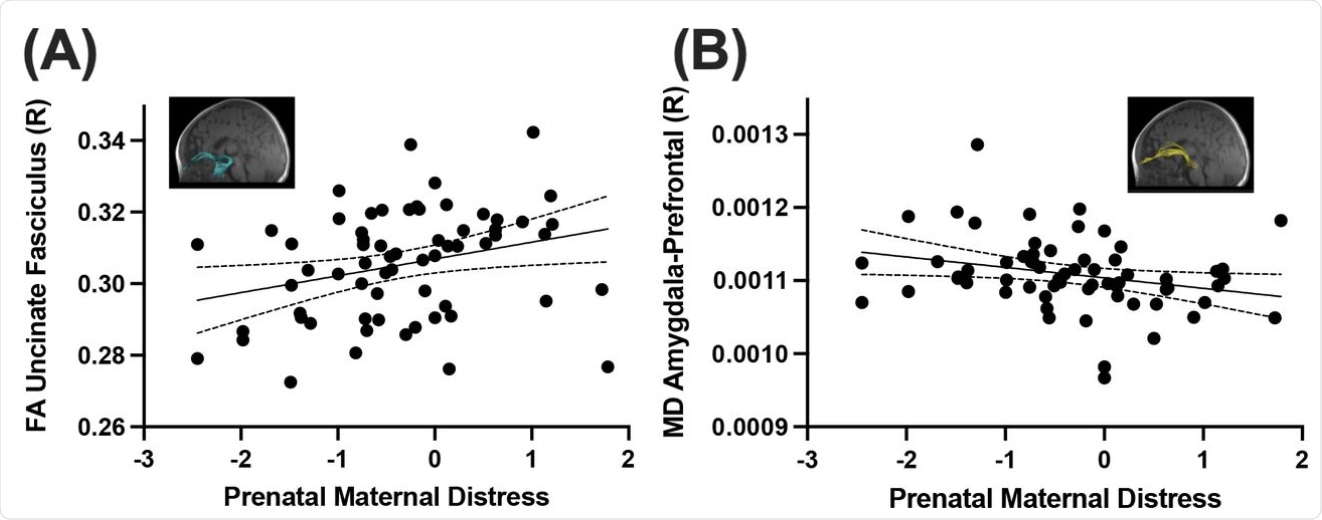 Prenatal maternal distress was significantly positively correlated with average fractional anisotropy (FA) in the right uncinate fasciculus (A), and negatively correlated with mean diffusivity (MD) in the right amygdala-prefrontal tract (B).
Prenatal maternal distress was significantly positively correlated with average fractional anisotropy (FA) in the right uncinate fasciculus (A), and negatively correlated with mean diffusivity (MD) in the right amygdala-prefrontal tract (B).
The infant brain structure was assessed on brain magnetic resonance image (MRI) scans at three months of life. The mothers of these babies had mean EDPS and PROMIS Anxiety scores which were lower than in the full sample but higher than pre-pandemic levels.
The scans showed that maternal prenatal distress affected mainly the right amygdala and the orbitofrontal cortex on the right side. Pregnant women with poor social support had a relationship between prenatal distress and reduced functional connectivity, but not those with good support.
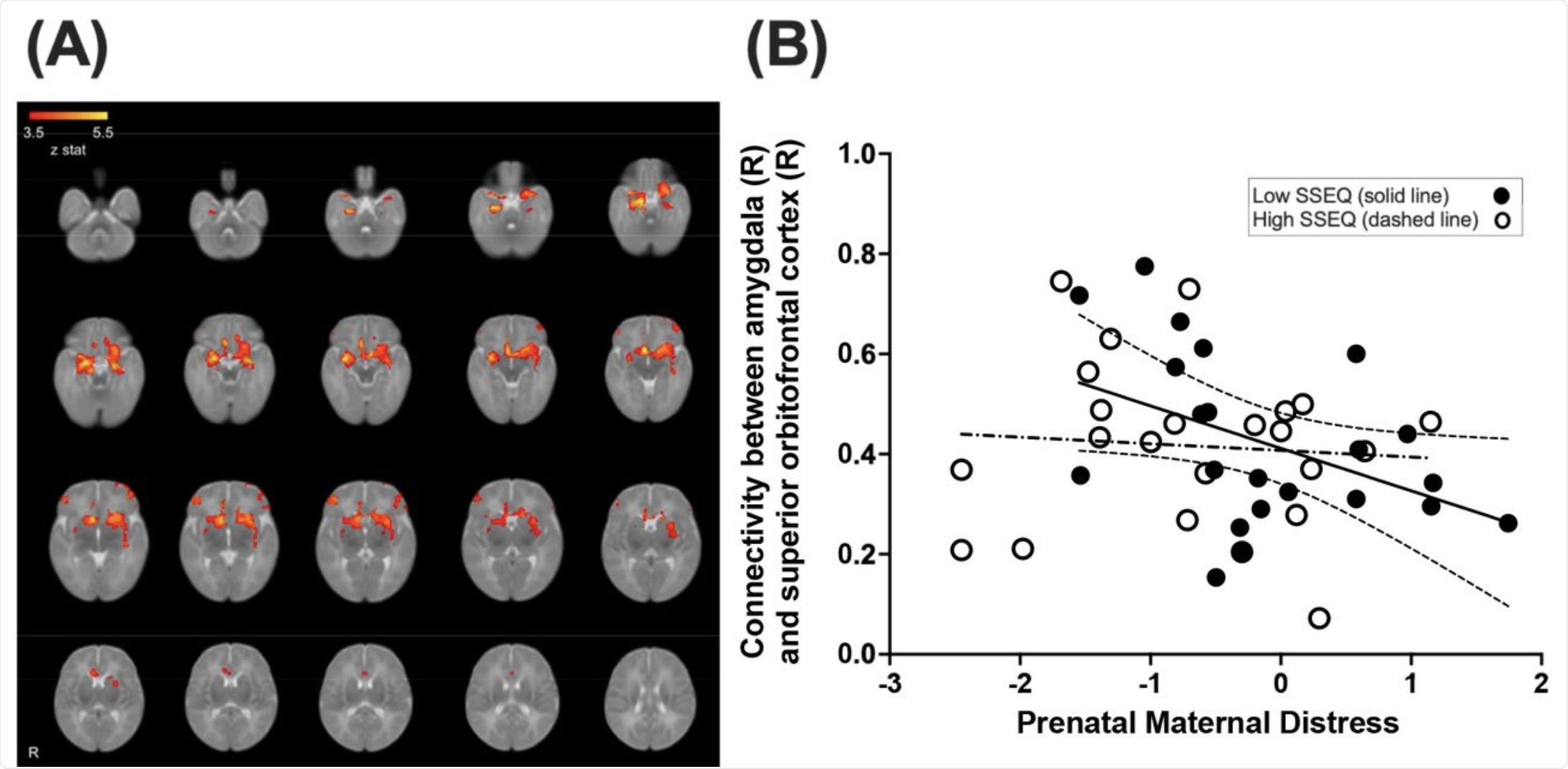 Average whole-brain functional connectivity of the amygdala is shown in infants (A). Functional connectivity from the right amygdala and the right superior orbitofrontal cortex demonstrated a significant interaction between SSEQ and prenatal maternal distress (B). The low SSEQ group demonstrated a significant negative correlation between maternal distress and connectivity (solid line) and the high SSEQ group did not (dashed line).
Average whole-brain functional connectivity of the amygdala is shown in infants (A). Functional connectivity from the right amygdala and the right superior orbitofrontal cortex demonstrated a significant interaction between SSEQ and prenatal maternal distress (B). The low SSEQ group demonstrated a significant negative correlation between maternal distress and connectivity (solid line) and the high SSEQ group did not (dashed line).
Implications
The results from this large study of pregnancy in Canada during the COVID-19 pandemic indicate a markedly higher rate of prenatal distress in mothers that were linked to alterations in the structure and function of the brain of their infants. Depression was identified in a third of mothers, and anxiety in almost half, during pregnancy.
Notably, the occurrence of distress among mothers was mitigated by proper social support, which dampened feelings of anxiety and depression. Whereas the functional connectivity of the brain was altered, as shown by the altered white matter connectivity, along with changes in the amygdala, social support prevented these changes.
This seems to show that providing social support to mothers is important, not only to support mothers but to reduce the resulting harm to the infant by modulating the transference of the mother’s prenatal distress via changes in the infant's brain.
The findings correlate well with earlier studies that show mothers who feel supported deal with psychological stress better than those who lack such support. Especially during the pandemic, people were separated for long periods of time from family and friends. Furthermore, individuals largely suffered from the absence of ordinary community interactions because of the restrictions on social gatherings, going out in public places, school/business closures, as well as travel bans.
In pregnancy, this meant that pregnant women were often forced to attend their prenatal appointments alone, and these were often switched out to virtual rather than face-to-face appointments. Sometimes the doctor or midwife responsible for the patient’s care was changed, which engendered anxiety and depression in the pregnant woman.
The altered amygdala-prefrontal cortex connectivity in infants born during the pandemic was shown in this study to be linked to maternal prenatal distress. The changes, which were seen on MRI scans of the brain in infants, may be interpreted as a precocious development of the white matter connections between the right amygdala and the prefrontal white matter, which are essential for regulating emotions.
Such changes in the right hemisphere white matter are linked to maternal depression in the prenatal period, as well as depression or risk of depression in children and adolescents. This may indicate that “functional and structural brain alterations may be an underlying mechanism via which maternal prenatal distress can lead to increased risk of mental health difficulties in offspring.”
The major contribution of social support to reducing the impact of prenatal distress on the pregnant woman and also on the developing fetal brain is a prominent finding in this study. The reduced functional connectivity between the right amygdala and the superior orbitofrontal cortex was found to be a marker of greater prenatal distress.
In other words, the functional connectivity that is responsible for the ability to regulate emotions and make decisions develops in an altered fashion. This has been suggested by research in young children, though studies in six-month-old infants contradict this.
Overall, it appears to be important to provide social support and thus prevent the transmission of the mother’s prenatal distress to the infant via aberrant brain development. The structural differences observed with prenatal distress were, however, not mitigated by social support.
“It is possible that these relationships may change in later stages of development as the functional and structural connectome of the infant brain continues to develop and refine.”
The plasticity of the brain in infancy and early childhood indicates that using evidence-based interventions can successfully correct the negative effects of prenatal stress and improve the child’s behavior, as well as prevent future mental ill-health.
“This highlights the pressing need for prenatal mental health screening as well as policies that target improving social support, as we have demonstrated that this may support healthy infant brain development in early life.”
*Important notice
medRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Manning, K. Y., Long, X., Watts, D., et al. (2021). Prenatal Maternal Distress During The COVID-19 Pandemic and Its Effects on The Infant Brain. medRxiv. doi:10.1101/2021.10.04.21264536. https://www.medrxiv.org/content/10.1101/2021.10.04.21264536v1
Posted in: Child Health News | Medical Science News | Medical Research News | Women's Health News | Disease/Infection News | Healthcare News
Tags: Adolescents, Amygdala, Anxiety, Brain, Children, Coronavirus, Coronavirus Disease COVID-19, Cortex, Depression, Doctor, Healthcare, Hospital, Hyperactivity, Limbic System, Mental Health, Neurology, Pandemic, Pregnancy, Prenatal, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Stress, Syndrome

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article