Protein A is a 42KDa cell surface protein which is found on the cell walls of 90% of Staphylococcus aureus bacterial strains. It is encoded for by the polymorphic X-region of the SpA gene, and functions as an immunoglobulin-binding protein, risperdal result characteristically being able to bind with the ‘Fc-region’ of IgG (immunoglobulin G). This protein is an integral part of the evolution of Staphylococcus aureus, as it can simplifies bacterial transmission, and allows it to take hold of the host in a shorter space of time.
What does Protein A do?
The main function of Protein A within the cell wall of S. aureus bacteria involves the host’s immune system. It is a virulence determinant (a molecule which determines how easily a pathogen can cause disease in a host) and plays a role in suppressing host B-cell responses – which therefore assists in preventing the host immune response from damaging the bacteria.
Protein A also binds to the ‘Fc region’ of IgG, and also to the ‘Fab regions’ of B-cells – triggering processes which ultimately block opsonophagocytosis, and kills the B-cells that it comes in contact with.
An experiment performed in 2015 showed that guinea pigs which were purposely infected with the S. aureus bacterial strain called SpAKKAA showed increased anti-S. aureus immune response. Immunisation with the SpAKKAA strain can be used to elicit the production of neutralizing antibodies – enabling the guinea pigs to develop sufficient protective immunity.
How does Protein A affect humans?
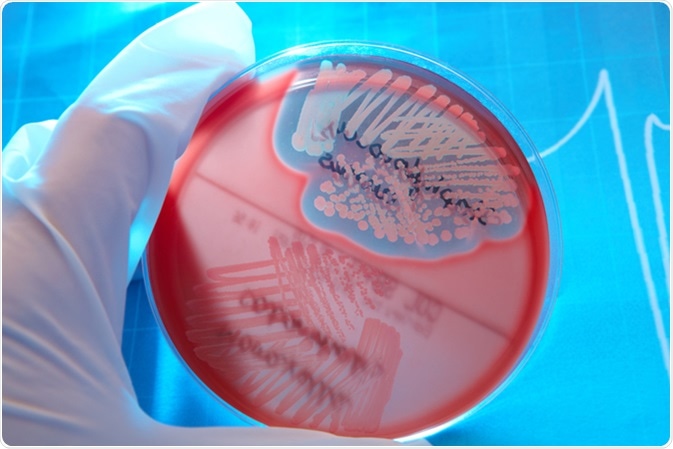
S. aureus is a Gram-positive and cocci-shaped bacterium, meaning that it appears purple with ‘Gram stain’, and these bacterial are seen as clusters of small, spherical cells. S. aureus is a part of the human microbiome – mostly being found on the surface of the skin and all mucous membranes (e.g. eyes, mouth and ears). They are opportunistic bacteria, meaning that if a break in the skin occurs, or if the host becomes immunodeficient in some way, S. aureus can eventually cause an infection.
When S. aureus does infect a human host, it may result in a variety of different diseases, but very commonly it causes recurrent soft tissue and skin infections. These infections have become more prevalent in recent years, mainly as nosocomial forms, as methicillin-resistant strains of S. aureus (MRSA) have evolved in hospitals across the western world.
In humans, protein A (once it is released into the extra-cellular environment) can bind with the ‘Fc’ fragment of immunoglobulin G (IgG) and has been observed to be antiphagocytic in vitro – which is consistent with its IgG binding abilities, as binding to IgG can interfere with bacterial attachment by the antibody. This means that it can prevent itself from being destroyed by certain elements of the human immune system (as was also similarly observed in the guinea pig experiment from 2013). S. aureus infections, such as endocarditis, are usually treated with a strong course of antibiotics.
Protein A can therefore function slightly differently in different species, but always has the same goal: it interferes with the host’s B-cells within their immune system to prevent S. aureus from being phagocytosed and destroyed. This is an ideal adaptation, and when coupled with the known propensity of S. aureus to be more easily transmitted than other coagulase-positive bacteria, it indicates faster and more widespread bacterial transmission.
Sources
- Staphylococcus aureus Protein A Promotes Immune Suppression
- Protein A Suppresses Immune Responses during Staphylococcus aureus Bloodstream Infection in Guinea Pigs
- Nontoxigenic protein A vaccine for methicillin-resistant Staphylococcus aureus infections in mice.
- Evaluation of recent Protein A stationary phase innovations for capture of biotherapeutics
- Effect of Protein A on Staphylococcal Opsonization
- Significance of Protein A Production by Staphylococci
- Molecular typing of methicillin-resistant Staphylococcus aureus on the basis of protein A gene polymorphism
- Staphylococcus Aureus
Last Updated: Feb 26, 2019
Written by
Phoebe Hinton-Sheley
Phoebe Hinton-Sheley has a B.Sc. (Class I Hons) in Microbiology from the University of Wolverhampton. Due to her background and interests, Phoebe mostly writes for the Life Sciences side of News-Medical, focussing on Microbiology and related techniques and diseases. However, she also enjoys writing about topics along the lines of Genetics, Molecular Biology, and Biochemistry.
Source: Read Full Article