For generations, the medical community has used the “standard human”—a 70-kilogram male—to guide education, research and practice. This means that for many conditions, although the recommended type, dosage and duration of treatment may be effective for the group of males who happen to weigh close to 70 kg, they might be far from optimal for most of the population, including all females.
In cancer, multiple bodily factors contribute to how the disease develops, progresses and responds to treatment, and many of these factors relate to sex.
Sex differences in cancer are not technically a new insight, but they have historically been somewhat overlooked. However, researchers have recently started to uncover some of the mechanisms behind how a person’s sex affects their experience of cancer. The realization that such knowledge may one day make it possible to improve outcomes for all patients has given more scientists the impulse to delve deeper into this area of research.
Many sex-based differences are relevant to cancer and its treatment
The anatomical differences between males and females are well known. Not only do males have different sex organs to females, but they also typically have higher muscle and bone mass, a lower fat mass and a visibly different skeletal shape. Males also have a higher body water content, which, alongside differences in metabolism and fat mass, can affect how the body responds to and breaks down cancer-killing drugs.
Some of these differences are due to males having one Y chromosome and one X chromosome, rather than the two X chromosomes in the female body. In fact, research suggests that genetics plays a very significant part, indicating that up to one third of the genome might be expressed differently by males and females.
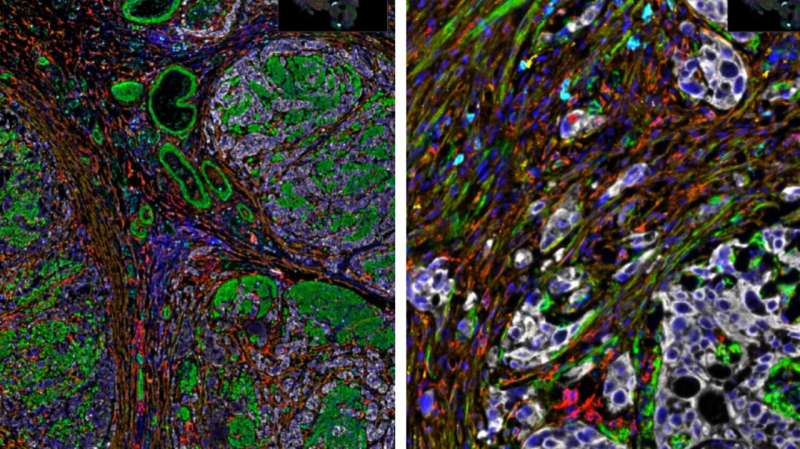
Females and males also have different sex hormones, and these influence the blood vessels, immune cells, signaling molecules and other features that surround tumors, known as the tumor microenvironment. For types of cancer that are dependent on or sensitive to hormones, these chemicals can promote the growth and spread of the disease.
Researchers have also uncovered differences between male and female immune responses. They believe that these are typically stronger in females, who tend to clear disease-causing organisms such as bacteria more quickly from the body and be better protected by vaccinations. Conversely, females are often more susceptible to inflammatory and autoimmune conditions, some of which are associated with an increased risk of cancer.
All of these differences mean that, although males are more likely than females to get cancer and to have a poor outcome, females are 34 percent more likely to experience side effects from cancer treatments, including chemotherapy, targeted therapy and immunotherapy.
Under-representation of females in clinical trials presents a barrier
A big part of the problem is that treatment recommendations are based on the findings of clinical trials, which are only generalizable if the trial participants are representative of the relevant patient population. This is an issue because females are generally under-represented in clinical trials.
For instance, between 2003 and 2016, females represented less than 10% of participants in lung and pancreatic cancer trials, despite accounting for more than 40% of the diagnoses. In 2018, women made up only 38% of the 5,157 people who participated in oncology trials that led to the approval of new drugs.
,The insufficient recruitment of female participants has historically been due to concerns that regular monthly hormonal fluctuations might affect the findings and that the intervention being tested could lead to fetal abnormalities in those capable of pregnancy.
Some gender-related misconceptions have also played a part. Research suggests some trial sponsors and clinicians believe that women bring complexity to clinical trials and that their ‘increased emotions and sensitivity’ may affect how they report their symptoms. However, these excuses are no longer considered valid.
Improved knowledge is key to driving change
For things to improve, it is crucial for scientists to develop a deeper understanding of the specific influences of sex differences in different cancer types.
Researchers at The Institute of Cancer Research recently contributed to a paper highlighting how sex affects incidence and outcomes in bladder cancer, published in Nature Reviews Urology.
Dr. Anna Wilkins, Clinical Scientist in the Division of Radiotherapy and Imaging’s Targeted Therapy team at the ICR and Consultant in Clinical Oncology at The Royal Marsden, and her colleagues decided to focus on bladder cancer partly because “it is generally a very neglected area” but primarily because of its “unusual nuance.” She explained:
“The difference between sexes seems to be most stark in bladder cancer, so it’s a good place to start. The prevalence is higher in men, but the outcomes are worse in women. The data are really striking.”
The difference in prevalence
Bladder cancer is about four times as common in males as in females, which cannot be solely due to behavioral differences. Although some of the key risk factors for the disease—smoking and exposure to chemical dyes—used to be more associated with males, the data no longer support this link.
The team’s paper covers a wide range of areas that need investigating in order to uncover why the outcomes for this cancer type are typically worse in females. This is challenging because the discrepancy in prevalence makes it harder to recruit women into clinical trials, resulting in less data.
An obvious starting point, therefore, is to try to determine how much of the difference in prevalence is actually due to a lack of diagnosis in females, for which biology is partly to blame.
When females present with blood in the urine—a common symptom of bladder cancer—clinicians are likely to assume that they have a urinary tract infection (UTI). The tube through which urine leaves the body is shorter in females, so it is easier for bacteria to enter the bladder. This means that UTIs are much more common among females than males.
“The issue is compounded by the fact that UTIs and bladder cancer can coincide,” Dr. Wilkins noted. “So if clinicians test for a UTI and find one, they don’t necessarily follow up to check for bladder cancer. We need greater public health awareness so that clinicians don’t only check for UTIs.”
The difference in outcomes
Researchers will also need to investigate why outcomes are worse in females. Is it just due to diagnosis occurring at a later stage, when treatment is less likely to be effective, or are there other factors at play?
Dr. Wilkins believes that scientists should focus on immunology, as male and female hormones have quite different immunological effects.
“Sex-specific immunological changes are important to investigate because they dictate how the genomics of tumors evolve and how cancer learns to escape the immune response,” she said. “This research has already proven fruitful in other cancers—for example, we use the reduction of testosterone levels as a first-line treatment for prostate cancer.”
Scientists also need to ensure that they have sufficient data to understand how best to treat males and females with bladder cancer. This might mean analyzing sex-specific data and differences, which will require clinical trial designers to purposefully incorporate differences into the design and reporting of clinical trials.
Dr. Wilkins was keen to stress that this research can benefit everyone, not just women. She said, “If we can start understanding why these differences exist, we can hopefully improve our understanding of the disease. Unpicking in detail why there are these disparities might lead to new research avenues in bladder cancer that are not linked to sex.”
Looking beyond bladder cancer
The authors of the paper are hopeful that their work will widen the avenue of research across all cancer types. As well as potentially improving patient outcomes through better diagnostics and treatments, this could reduce the burden that cancer places on the health system.
Dr. Anna Wilkins concluded, “We’ve made so much progress in uncovering the myriad of factors that can affect a person’s likelihood of getting cancer and influence how they respond to treatment. We’ve known for a long time that internal factors—a person’s genes, immune function and hormones—are just as significant as external ones in some cancer types, and we know of hundreds of biomarkers that help clinicians understand a person’s specific tumor biology. Yet many of the sex gaps in cancer incidence and outcomes remain something of a mystery.
“We can’t stall any longer—we need to answer as many of the outstanding questions as possible so that we can improve the lives of all people with cancer.”
More information:
Paul Toren et al, The sex gap in bladder cancer survival—a missing link in bladder cancer care?, Nature Reviews Urology (2023). DOI: 10.1038/s41585-023-00806-2
Journal information:
Nature Reviews Urology
Source: Read Full Article