Biliary atresia is a relatively rare childhood condition affecting the liver, with the potential to inflict hepatocellular damage or liver failure if left untreated. While the condition affects about 0.42 to 2.9 per 10,000 infants, prevalence rates differ across geographies.
Rapid surgical intervention is the cornerstone of life-saving treatment and can be effectively administered with early detection of the disease in infancy. Currently, early detection methods like the stool color card and direct bilirubin (DB) concentration test are used for screening newborns and have demonstrated cost-effectiveness and potential life-saving benefits.
Unfortunately, studies gauging the cost-effectiveness of these methods have largely focused on low disease prevalence countries, leaving out countries like Japan, which have a comparatively higher prevalence rate.
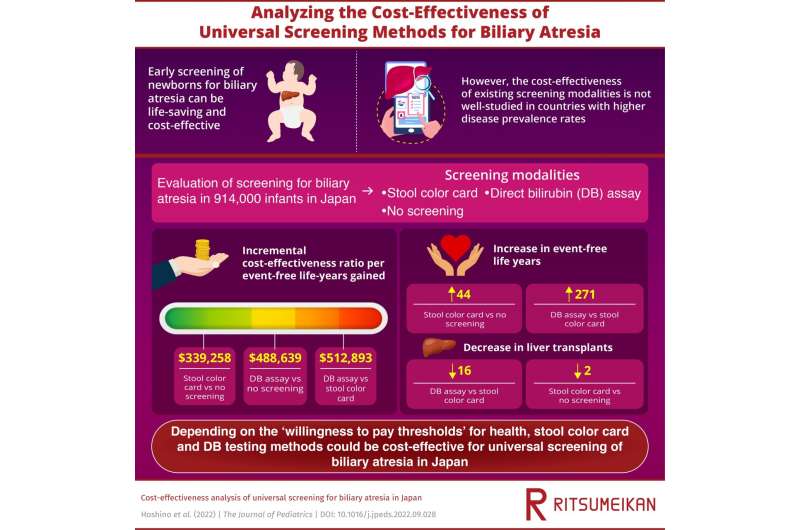
Expanding this evaluation to countries with higher prevalence rates, a team of researchers from Japan, led by Associate Professor Eri Hoshino of Ritsumeikan University set out to study the cost-effectiveness of the existing universal screening methods for biliary atresia in Japan. In their study, published in The Journal of Pediatrics, the researchers looked at the cost-effectiveness of both the stool color card method, and the DB test and compared it to no screening option.
Talking about their research, Dr. Hoshino said, “Early screening for biliary atresia has significant clinical benefits, and timely intervention, especially before the age of 30 days, can be life-saving. Yet, no study has looked at the cost-effectiveness of these methods in Japan which has higher prevalence rates.”
To this end, the researchers used a Markov microsimulation model to simulate the intervention outcomes in a cohort of 941,000 newborns with the three strategies. This helped determine event-free life-years, or liver transplant-free life-years, costs, and incremental cost-effectiveness ratio (ICER) over a 25-year period. They performed both base case as well as scenario analysis to capture a holistic picture of the cost-effectiveness with early diagnosis of the condition.
In the base case analysis, the researchers simulated a scenario of intervention within 45 days of birth after screening. They found that universal screening using stool color card helped gain 44 event-free life-years compared to the no screening method and resulted in 2 fewer liver transplants. While this translated into an ICER of $339,258 per event-free life-year gained, DB screening yielded an ICER of $488,639 per event-free life-year gained, when compared to no screening.
Moreover, universal screening using DB test added 271 more event-free life-years with an ICER of $512,893 compared to the stool color card method. Notably, it also prevented 16 liver transplants compared to the stool color card method.
These results improved slightly during the scenario analysis, which was simulated to target optimal intervention within 60 days of birth.
Explaining the relevance of these results, Dr. Hoshino says, “In general, cost-effectiveness is found by comparing ICER to a threshold value called the Willingness to Pay (WTP) value. In Japan, currently the threshold is around $33,000 (or 5 million Japanese Yen) per quality-adjusted life-year.
“The low-incidence and life-long treatment for conditions like biliary atresia makes it look like the screening methods are not cost-effective. Yet, for evaluating conditions like these, the WTP must be raised higher. Thus, compared to the proposed higher WTPs for ultra-rare cases, both the screening methods are seen to be cost-effective with improved efficiencies.”
The researchers also speculate that different dissemination path for methods like stool color card test in Japan may be responsible for higher costs, and suggest that utilizing mobile apps can help bring these costs down. Moreover, combining universal screening for biliary atresia with screening for other diseases can further optimize these costs.
With the risk of demographic changes in Japan looming large, prioritizing infant health care can increase healthy life expectancy of the infant population. Assessments like these can provide policymakers the much-required evidence to implement the necessary health policies.
As Dr. Hoshino rightly concludes, “By providing a comparison of different screening strategies in terms of costs and consequences, the results of this study can eventually guide the national screening guidelines and translate into healthier lives for affected patients.”
More information:
Eri Hoshino et al, Cost-effectiveness analysis of universal screening for biliary atresia in Japan, The Journal of Pediatrics (2022). DOI: 10.1016/j.jpeds.2022.09.028
Journal information:
Journal of Pediatrics
Source: Read Full Article