According to a recent study, German kids with type 1 diabetes (T1D) across the socioeconomic spectrum are now using technology to control their glucose levels better than they did a decade ago. Meanwhile, young, impoverished Americans with T1D are doing worse. That’s because children receiving T1D care in the United States face a technology divide between the haves and the have-nots, says Ananta Addala, assistant professor of pediatrics at Stanford Medicine Children’s Health. “We’re not improving outcomes for our poorest youth.”
What drives this disparity? The bureaucratic hassles of public insurance (i.e., Medicaid) can make it difficult for patients to obtain continuous glucose monitors and use them without interruption. In addition: Providers are reluctant to deal with those hassles. “Provider bias against public insurance is a problem in technology recommendation,” Addala says.
To address this problem, Stanford University researchers initiated the 4T Program, a clinical research study to determine whether baking equity into intensified diabetes management for children can improve their long-term outcomes. A key piece of the program (and one of the four T’s) is technology: Every young person diagnosed with T1D is offered a continuous glucose monitor (CGM) within one month of diagnosis, as well as education on how to use it. Their glucose levels are also monitored remotely, with an AI system determining which patients should be prioritized for a dose adjustment by the clinician education team. The goal: tight control of patients’ glucose levels within specified targets.
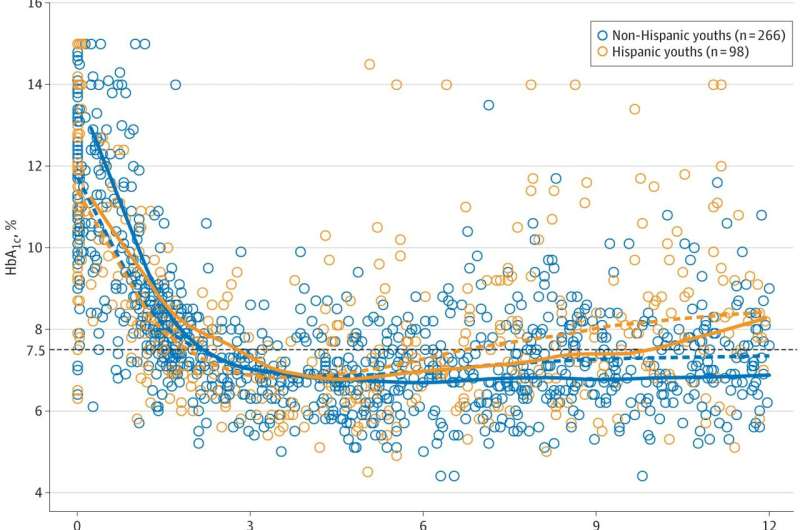
The results of the 4T Program’s pilot study have been published in JAMA Network Open. They reveal that key measures of wellness for youth with diabetes improved dramatically for 4T Program participants across the socioeconomic spectrum, although Hispanic youths and those on public insurance still lag behind their counterparts.
An additional lesson: Remote monitoring also improves outcomes, but it only works if patients are provided with continuous cloud connectivity and a smart device. “To achieve health equity, we need to close the digital divide,” Addala says.
The 4T Program
Endocrinologists have known that intensive management of T1D helps keep patients’ glucose levels on an even keel. And continuous glucose monitors, which measure glucose levels every 5 to 15 minutes, have made it easier for patients to hit their glucose level targets more consistently.
CGMs can also be remotely monitored, allowing clinicians to track the percentage of time patients’ levels are within the target range—a figure known as “time in range.”
The 4T Program was designed with equity in mind, Addala says. For example, she and her colleagues knew that publicly insured patients with T1D suffer worse outcomes due to insurance-related interruptions in CGM availability. They therefore made sure all participants had continuous access to CGMs regardless of their insurance status, and within one month of diagnosis. “We uncoupled the payor factor by guaranteeing that people could have immediate and uninterrupted access to CGMs,” she says.
Similarly, all participants were remotely monitored by a system that continuously calculates patients’ time in range and then uses an AI algorithm to prioritize which patients should receive additional outreach from clinical educators. It’s an efficient way to preempt a change in glucose levels that might otherwise result in a three-hour clinic visit, Addala says. “We’re providing better health care because we’re preventing adverse outcomes, and we’re also using clinical resources more efficiently.”
And the results bear this out: Across the socioeconomic spectrum, 4T Program participants had better glycemic control than a historic cohort that didn’t have access to continuous glucose monitoring. In addition, patients with remote monitoring had slightly better glycemic control over the course of the 12-month study than those without.
But there is a caveat: “Providing technology to kids with type 1 diabetes improves glucose levels for everyone, but those who are on public health insurance or are members of historically minoritized groups still lag behind their counterparts,” Addala says. As she sees it, technology alone can’t entirely overcome certain social determinants of health such as language barriers and fluency in the use of online resources.
The digital divide and remote monitoring
The team also bumped into another challenge for those seeking to reduce health disparities: the digital divide.
When the 4T Program team first provided remote monitoring to study participants, the data suggested that many of the patients who rely on public insurance as well as those who are members of historically minoritized groups weren’t consistently wearing their monitors. But this result seemed peculiar to the study team.
“People wear their CGMs,” Addala says. “And in equity research, if a story doesn’t quite add up, you need to dig into the data.” As it turned out, the devices used by the less economically advantaged study participants weren’t maintaining consistent internet connectivity. So, a few months into the pilot program, the team pivoted to offering smart devices and reliable WiFi access to all patients.
Next steps
With the 4T Program’s pilot study complete, the team is about to wrap up data collection for a larger study in which all participants received both CGMs and remote monitoring. And in a second study, which has also begun, participants are being offered both CGMs and insulin pumps. The goal: to get youths with T1D exposed to pumps in a systematic manner and also to integrate the 4T remote monitoring algorithm with the automated algorithms that are part of the pump and sensor.
The team is also disseminating the 4T Program to other hospitals including Children’s Mercy Hospital in Kansas City.
“We want to learn what another clinic might need that’s not Stanford,” Addala says. “That is absolutely next on the horizon.”
More information:
Ananta Addala et al, Disparities in Hemoglobin A1c Levels in the First Year After Diagnosis Among Youths With Type 1 Diabetes Offered Continuous Glucose Monitoring, JAMA Network Open (2023). DOI: 10.1001/jamanetworkopen.2023.8881
Journal information:
JAMA Network Open
Source: Read Full Article