Effective tuberculosis (TB) treatment has been available for the past 60 years. But TB remains the leading cause of death from a single infectious agent. It ranks above HIV and AIDS and others. This is partly because of the impact of HIV co-infection among TB patients in places like Africa and emergency of MDR-XDR TB. Lack of both gender mainstreaming and reduction of stigma manifested by persistently lower reported cases among women that men is of continued concern.
COVID-19 surpassed TB as a killer over the past two years. The number of people dying from TB have been going down since 2005. But now TB is again at number one. Between 2019 and 2021 the number of people provided with treatment for TB decreased—largely due to COVID-related lockdowns. In 2021, 61% of people with TB were receiving treatment, this is lower that 69% in 2020.
What went wrong?
Progress in TB elimination was being made. But the COVID-19 pandemic and associated lockdowns have set back TB control programs worldwide. More so in Africa. While COVID-19 prevention measures like mask-wearing could have prevented TB transmission, on the whole, little attention was given to holding the forts of TB prevention and treatment as all efforts went to fighting the COVID-19 pandemic, disrupting well-functioning programs built over decades of careful research and planning. This disruption has resulted in the following:
a) Increased TB cases:
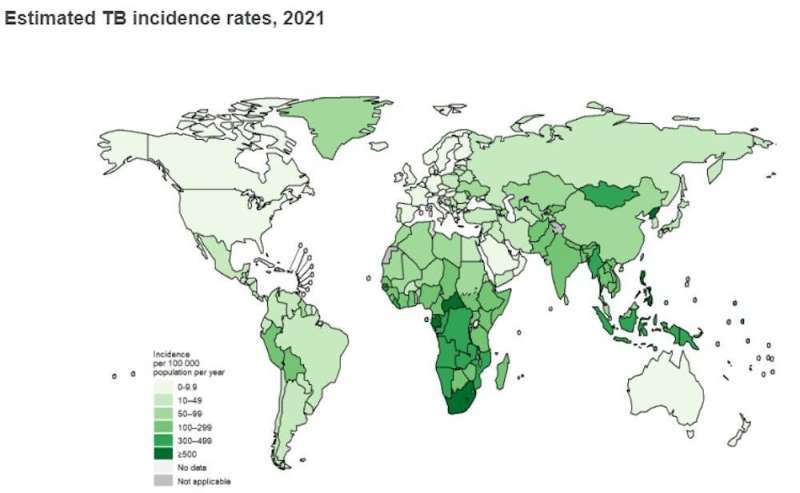
In 2021, there were 10.6 million new active TB cases worldwide: up from 9.9 million in 2020. These increases have been in both drug sensitive and multi-drug resistant TB cases.
b) Increased TB deaths:
In 2021 there were an estimated 1.6 million deaths from TB worldwide: up from 1.5 million in 2020 and 1.4 million in 2019. This is a reversal of years of decline before the COVID-19 pandemic. A quarter (25%) of TB related deaths occur in the African region which has around 16% of world’s population. HIV being a main contributing factor.
c) Decline in TB global spending during and after COVID-19 pandemic:
Global spending on essential TB services dropped from US$6.0 billion in 2019 to US$5.4 billion in 2021. This is less than half of what is needed. The war in Ukraine has compounded this extended decline in TB prevention and control. Even before the Russian invasion, Ukraine had a high TB rate. The war has exacerbated the situation with health facilities being destroyed and people displaced. African TB control programs that rely on aid and Global Fund support have been affected most.
How do we correct this?
The first End TB Strategy milestones for reductions in TB disease should guide what needs to be done. This includes 20% reduction in 2015 TB incidence rates, and 35% reduction in total number of TB deaths benchmarked in 2015. Three high TB burden countries in Africa have reached or passed the first milestones of the End TB Strategy for both reductions in TB incidence and TB deaths: Kenya (in 2018), Tanzania (in 2019) and Zambia (in 2021). Ethiopia is very close. However, the larger part of the African continent has seen a reversal in gains made.
Intensified efforts to obtain funding are urgently required to mitigate and reverse the negative impacts of the COVID-19 pandemic on TB. This has become even more pressing in the context of ongoing conflicts in Africa and other parts of the world, which are likely to worsen some of the broader determinants of TB such as undernutrition.
Priorities for TB care should be:
-
Increase budget and human resources for existing TB and TB/HIV services
-
Develop digital platforms for training and health education. Develop public-facing dashboards for TB surveillance data. Develop telemedicine with the use of digital platforms for consultation. Reduce loss to follow up
-
Strengthen community-based TB treatment services
-
Scale up virtual care, community-monitoring solutions to provide remote support such as video-supported therapy. Scale up SMS-based communication to improve treatment adherence and patient-centered care and support
TB prevention should focus on:
Target high-risk groups for universal testing, to find most or all missing active TB cases in communities
Strengthen community-based active case finding and tuberculosis diagnostic services (including in shelters for people who are homeless).
Integrate TB, HIV and COVID-19 services including screening and testing, case finding and prevention.
Enhance screening and case finding activities at health facilities, including targeting high-risk groups
Increased screening for TB in high-risk groups. Use rapid turnaround molecular tests with high sensitivity and specificity for dual diagnostic testing for TB and COVID-19
Expand use of chest radiography with or without computer-aided detection for TB, and improve facility-based screening
Ensure regular supply of diagnostics and drugs through local manufacturing.
Provided by
The Conversation
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Source: Read Full Article