As demand for shoulder replacement surgery grows, a new study finds that up to 1 in 6 patients are having to travel to a different region for surgery, and exposes a year on year increase in the risk of serious adverse events after surgery that require admission to hospital.
Shoulder pain can significantly impact a person’s quality of life, and for many individuals with severe joint arthritis, shoulder replacement surgery offers a promising solution. However, a new study conducted by researchers at NDORMS, University of Oxford, and published in BMC Medicine, highlights concerning trends in the availability of and outcomes after shoulder replacement surgery in England.
The researchers examined data from all elective shoulder replacements carried out by NHS hospitals and NHS-funded care in England from 1999 to 2020 to evaluate service provision and assess patient outcomes including serious adverse events and revision surgery.
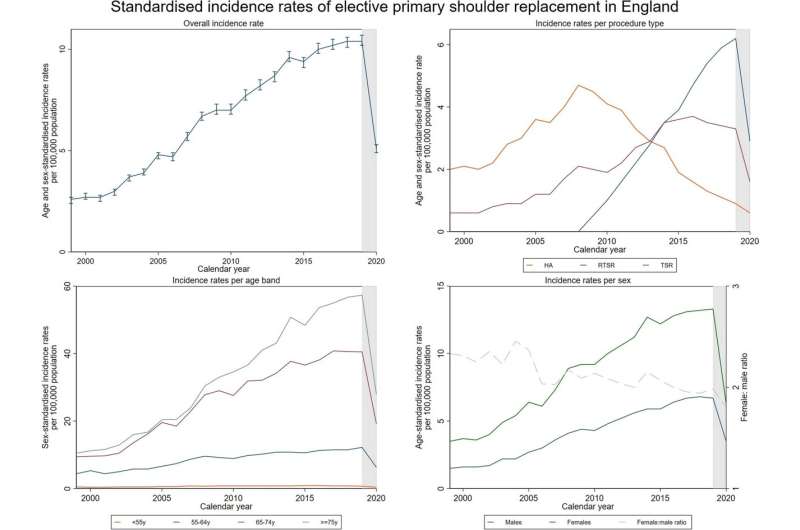
During that period there was a significant increase in the number of shoulder replacement surgeries performed in England. In fact, the incidence of primary shoulder replacements quadrupled from 2.6 to 10.4 per 100,000 population. Patients aged over 65 contributed the most to this increase.
Epaminondas Markos Valsamis, NIHR Doctoral Research Fellow at NDORMS said, “We saw that the incidence of elective shoulder replacement surgery has increased rapidly over the last 20 years and is expected to more than triple by 2050, with associated hospital costs expected to reach £235 million. However, our study highlighted considerable inequality in service provision across the country meaning that up to 1 in 6 patients from the East Midlands had to travel to a different region to get their surgery.”
The study showed that disparities in access to shoulder replacement surgery sat alongside an increase in the incidence of serious adverse events (SAEs) associated with shoulder replacement surgery. The risk of SAEs within 30 days rose from 1.3% to 4.8%, while the risk within 90 days increased from 2.4% to 6.0% over the study period, which was alarming. Additionally, patients from more deprived socioeconomic groups appeared to have a higher risk of SAEs and revision surgery.
“A key aim of this study was to forecast future patient demand for shoulder replacement surgery in England and the results serve as a valuable contribution to the ongoing discussions surrounding health care provision and access to elective surgery,” said Markos. “While the COVID-19 pandemic exacerbated the already rising waiting times for elective surgery, these findings highlight the workforce planning that will be needed to address the growing demand while ensuring that everyone has equal access to surgery regardless of where they live.”
More information:
Epaminondas Markos Valsamis et al, Shoulder replacement surgery’s rising demand, inequality of provision, and variation in outcomes: cohort study using Hospital Episode Statistics for England, BMC Medicine (2023). DOI: 10.1186/s12916-023-03112-1
Journal information:
BMC Medicine
Source: Read Full Article