Some HIV-1 carriers who have received an early antiretroviral treatment during several years are able to control the virus for a long term after treatment interruption. However, the mechanisms enabling this post-treatment control have not been fully elucidated.
For the first time, teams of scientists from the Institut Pasteur, Inserm and the Paris Public Hospital Network (AP-HP), supported by ANRS | Emerging Infectious Diseases, have investigated and revealed how neutralizing antibodies, including those described as broadly neutralizing, contribute to virus control. These key findings were published in the journal Cell Host & Microbe.
“Post-treatment controllers” is the term used to describe the rare HIV-1 carriers who, having initiated treatment early and maintained it for several years, are able to control the virus for years after that the treatment has been discontinued. These individuals were identified several years ago in part through the VISCONTI study, which assembled the largest cohort of long-term post-treatment controllers in France.
Although the mechanisms of viral control enabling the long-term remission from HIV-1 infection without antiretroviral therapy have not been fully elucidated, the identification of these cases provides a unique opportunity to refine our understanding of the factors associated to HIV-1 infection control.
A study conducted by the Institut Pasteur’s Humoral Immunology Unit led by Dr. Hugo Mouquet in collaboration with the team led by Dr. Asier Sáez-Cirión, Head of the Institut Pasteur’s Viral Reservoirs and Immune Control Unit, is now contributing to efforts to describe these mechanisms in more detail. Asier Saéz-Cirión explains: “Our investigation published in 2020 on the immune response in post-treatment controllers marked a major first step in demonstrating an effective and robust antibody response to HIV-1 in some of these individuals, which may contribute to this control.
This knowledge has now been further advanced by our new study. By investigating the role of antibodies in a specific “post-treatment controller” case with particularly high serum levels of broadly neutralizing antibodies, we discovered that remission was probably linked to the activity of this type of antibodies.”
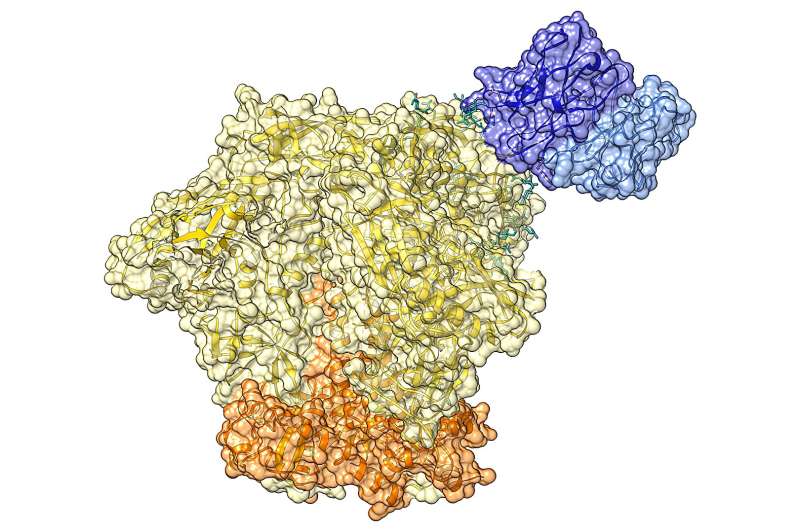
Hugo Mouquet describes the discovery: “Our study describes for the first time in a post-treatment controller a family of broadly neutralizing antibodies (bNAbs) targeting the HIV-1 envelope protein, of which the antibody EPTC112 is one of the most active member.”
The antibody EPTC112 neutralizes about a third of the 200 viral variants of HIV-1 tested in vitro and is able to induce the elimination of infected cells in the presence of natural killer (NK) cells, the immune cells eliminating abnormal cells in the body.
This study therefore provides important insights on how neutralizing antibodies modify the course of HIV-1 infection in this individual from the VISCONTI cohort. Although the HIV-1 virus circulating in this subject was found to be resistant to EPTC112 neutralization due to mutations in the region targeted by this antibody, it was effectively neutralized by other antibody populations isolated from the blood of the individual. Hence, the study suggests that neutralizing antibodies from the EPTC112 family impose a selective pressure on the HIV-1 virus.
Although the virus escaped the action of these bNAbs, it remained susceptible to the neutralization by other anti-HIV-1 antibodies produced in this individual. This observation suggests the existence of a cooperation between the various populations of neutralizing antibodies.
“The fact that we discovered a potential link between the production of neutralizing antibodies, including bNAbs, and the HIV-1 control is exciting to better understand the underlying mechanisms of viral control, particularly by studying additional post-treatment controllers with similar profiles. Indeed, we wish to continue investigating on a short term whether the antibody responses in other ‘post-treatment’ controllers also contribute to long-term remission from the infection,” explains Hugo Mouquet.
This discovery paves the way for new avenues of HIV-1 therapy and fuels hopes of therapeutic approaches for increasing the chances of remission without antiretroviral treatment through the use of broadly neutralizing antibodies. To this end, a clinical trial involving the administration of broadly neutralizing antibodies should begin in France before the end of 2023.
“This Phase II trial conducted by the ANRS RHIVIERA consortium through a partnership between the Institut Pasteur, AP-HP, Inserm and the Rockefeller University in New York, will investigate the combination of an antiretroviral therapy in the primary infection phase with two long-acting HIV-1 bNAbs versus placebo to determine whether these antibodies contribute to establishing viral remission after antiretroviral treatment discontinuation.”
“69 patients in the primary HIV-1 infection phase are planned to be enrolled. They will first receive a short-term antiretroviral treatment, followed by a therapy with the two bNAbs targeting two different regions of the virus envelope protein. It will be possible to stop therapy after a year of close monitoring based on a detailed set of criteria. This trial will enable us to determine whether this therapeutic strategy is able to induce a sufficient immune response to control the infection after the discontinuation of antiretroviral therapy,” concludes Hugo Mouquet.
More information:
Luis M. Molinos-Albert et al, Anti-V1/V3-glycan broadly HIV-1 neutralizing antibodies in a post-treatment controller, Cell Host & Microbe (2023). DOI: 10.1016/j.chom.2023.06.006
Journal information:
Cell Host & Microbe
Source: Read Full Article