A research team led by Prof. Dr. Tamam Bakchoul from the Institute for Clinical and Experimental Transfusion Medicine (IKET) at the University Hospital of Tübingen is investigating the suitability of anticoagulants in patients who develop thrombosis at unusual sites after vaccination against SARS-CoV-2. With the help of the study results, the scientists and physicians are hopeful to further explore new approaches to the treatment of this rare yet deadly condition. The study is now published in the journal Blood.
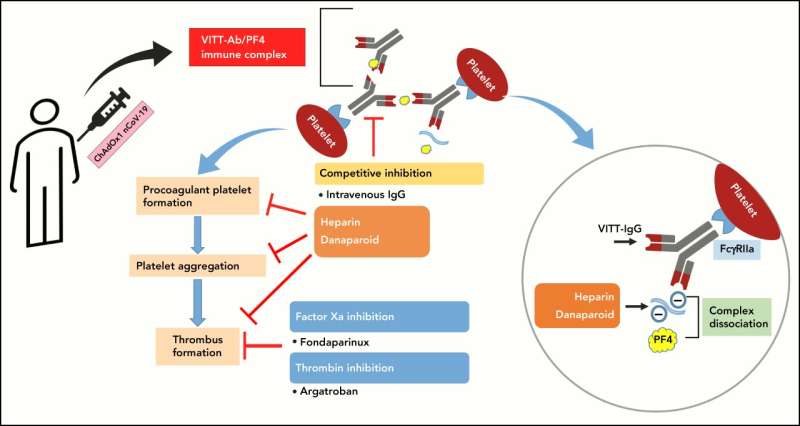
With the increasing number of vaccinations against the COVID-19 pandemic, reports of very rare but serious adverse side effects of vaccination have been presented. In some of the most severe cases, life-threatening thrombotic events occur at unusual sites. This condition is termed as vaccine-induced thrombotic thrombocytopenia (VITT). Heparin is usually preferred as one of the most widely used anticoagulants for prevention and treatment of thrombotic events due to its rapid action, low cost and availability. However, pathophysiology of VITT has been proposed to be similar to that of heparin-induced thrombocytopenia (HIT), and associated with platelet-activating antibodies against platelet factor 4 (PF4). HIT is defined as a complication of treatment with heparin, which results in a reduction in the platelet count, and a simultaneous tendency to thrombosis. Therefore, the use of heparin is discouraged in VITT patients to treat thrombosis because of similarities observed between VITT and HIT.
In the present study, Dr. Anurag Singh and team from Prof. Bakchoul’s group investigated the role of heparin and other anticoagulants in VITT. As part of a study, the scientists analyzed the binding between VITT antibodies and PF4, activation of platelets by serum from VITT patients and VITT-antibody-mediated thrombus formation. The results show that the interaction of heparin with VITT antibodies is not similar to that of HIT. Unlike HIT, heparin can inhibit thrombus formation in VITT patients, and in part through the inhibition of the interaction of VITT antibodies with PF4 and subsequent platelet activation. Prof. Bakchoul explains, “We were able to prove that these antibodies from VITT patients do not show the same effect as antibodies from HIT in presence of heparin. VITT antibodies did not show any increased binding with heparin, and the antibody-PF4 complexes were successfully dissociated by heparin.”
Source: Read Full Article