The skin is the largest organ in the human body and plays an important role in maintaining homeostasis as well as protecting the body from the outside environment. Skin diseases can be life-threatening or heavily impair patients’ quality of life. Urticaria (also called “hives”) is common, affecting at least one in five people in their lifetime, and can persist for years or even decades.
Many skin diseases are unique to humans, and their pathogenesis often remains unclear due to the lack of an appropriate experimental animal model and limited clinical data. One such human-specific disease is chronic spontaneous urticaria (CSU), which is characterized by the appearance of skin eruptions called wheals, which have a range of sizes and shapes and are accompanied by itching.
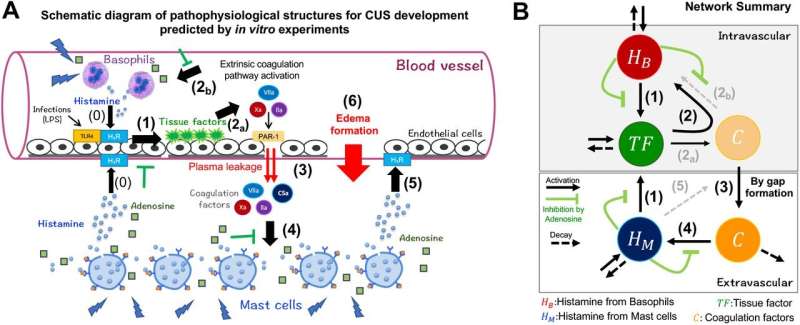
Despite CSU having a clear and visible appearance on the skin surface, the mechanism underlying the various shapes of wheals in vivo remains largely obscured. Recently, a number of pathophysiological characteristics of urticaria have been investigated, including autoimmune responses, cellular infiltrates, and activation of the coagulation pathway by the complement system. It is therefore of great importance to integrate these elements into their dynamics in vivo in order to develop more effective patient-specific treatments.
To address this, a research group led by Professor Sungrim Seirin-Lee at Kyoto University Institute for the Advanced Study of Human Biology (WPI-ASHBi) leveraged hierarchical mathematical modeling to analyze the shapes of skin eruptions and link these morphological features to the in vivo pathological dynamics of CSU. Their findings are published in Communications Medicine.
By incorporating both the intravascular and extravascular dynamics using in vitro experimental data, they classified the skin eruption patterns into five potential types.
Using these patterns, the researchers developed the Criteria for Classification of Eruption Geometry (EGe criteria) according to their relations with tissue factor and histamine dynamics of mast cells, which act on blood vessels and induce wheal formation.
The researchers then demonstrated the validity of their mathematical model to classify CSU according to these criteria in 105 patients, and found the reliability to be as high as 87.6% when analyzed by dermatologists.
“This study was the first to use mathematical models to clarify the pathophysiology of skin eruptions according to their morphology, and can help to pave the way for alternative treatment methods. For example, patients might take photos of their skin eruptions to provide data for a definitive diagnosis of underlying causes, or the effectiveness of treatment can be monitored over time. In addition, this study shows the promise of mathematical models in the understanding the mechanisms of human-specific diseases, where animal models are not available,” Seirin-Lee said.
Through these efforts, the authors hope to pioneer mathematical dermatology as a new multidisciplinary research field for practical use, integrating mathematical science and clinical dermatology for elucidating the pathophysiology of skin diseases and developing new strategies for managing intractable skin diseases.
More information:
Sungrim Seirin-Lee et al, Mathematical-based morphological classification of skin eruptions corresponding to the pathophysiological state of chronic spontaneous urticaria, Communications Medicine (2023). DOI: 10.1038/s43856-023-00404-8
Journal information:
Communications Medicine
Source: Read Full Article