Like the lymphatic system in the body, the glymphatic system in the brain clears metabolic waste and distributes nutrients and other important compounds. Impairments in this system may contribute to brain diseases, such as neurodegenerative diseases and stroke.
A team of researchers in the McKelvey School of Engineering at Washington University in St. Louis has found a non-invasive and non-pharmaceutical method to influence glymphatic transport using focused ultrasound, opening the opportunity to use the method to further study brain diseases and brain function. Results of the work are published in the Proceedings of the National Academy of Sciences on May 15.
Hong Chen, associate professor of biomedical engineering in McKelvey Engineering and of neurological surgery in the School of Medicine, and her team, including Dezhuang (Summer) Ye, a postdoctoral research associate, and Si (Stacie) Chen, a former postdoctoral research associate, found the first direct evidence that focused ultrasound, combined with circulating microbubbles—a technique they call FUSMB—could mechanically enhance glymphatic transport in the mouse brain.
Focused ultrasound can penetrate the scalp and skull to reach the brain and precisely target a defined region within the brain. In previous work, Chen’s team found that microbubbles injected into the bloodstream amplify the effects of the ultrasound waves on the blood vessels and generate a pumping effect, which helps with the accumulation of intranasally delivered agents in the brain, such as drugs or gene therapy treatments.
“Intranasal delivery provides a novel, non-invasive route to investigate the glymphatic pathway in intact brains,” Chen said. “This route for investigating glymphatic transport has the potential to be utilized in the study of glymphatic function in humans, which is currently limited by the absence of non-invasive approaches to access the glymphatic system.”
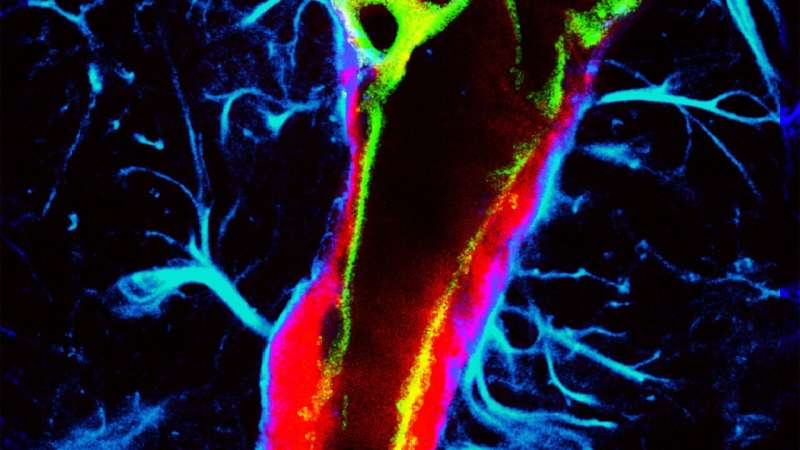
In the new research, the team administered a fluorescently labeled tracer intranasally. Then they administered focused ultrasound waves aimed deep in the brain at the thalamus after intravenous injection of microbubbles. When they conducted 3D imaging of the brain tissue on the treated side, they found that FUSMB boosted the transport of the tracer in the perivascular space.
They compared this with three control groups with various combinations of focused ultrasound, microbubbles and the tracer. All of the mice in the three control groups showed lower tracer accumulation, which verified to the team that the enhanced tracer transport was the result of the focused ultrasound with microbubbles.
To further validate their results, they used the FUSMB treatment after injecting the tracer directly to the cerebral spinal fluid, an invasive yet commonly used method. They found that FUSMB also enhanced the transport of tracers along the vessels at the focused-ultrasound targeted brain site by about two- to threefold compared with the non-targeted side.
“Regardless of whether tracers were delivered via the intranasal or injected route, FUSMB consistently improved glymphatic transport,” Ye said. “Our study using confocal microscopy imaging combined with brain-tissue clearing obtained direct evidence that unequivocally proved that FUSMB enhanced the glymphatic transport of a labeled protein agent in mice.”
The team also investigated various types of vessels, including arterioles, capillaries and venules, that facilitate FUSMB-enhanced transport of the tracer using both intranasal and injected delivery of the tracer. They saw improved glymphatic transport of the tracer in both arterioles and capillaries with both types of delivery. They found that the fluorescence intensity was higher along arterioles than capillaries and venules.
“This study opens new opportunities to use ultrasound combined with microbubbles as a non-invasive and nonpharmacological approach to manipulate glymphatic transport,” Ye said. “Focused ultrasound-activated microbubbles have the promise to enhance waste clearance in the brain and potentially mitigate brain diseases caused by impairments in glymphatic system function.”
Chen said the team will now focus on applying this non-invasive and non-pharmacological method for brain waste clearance to potentially combat neurodegenerative diseases, such as Alzheimer’s and Parkinson’s diseases.
More information:
Dezhuang Ye et al, Mechanically manipulating glymphatic transport by ultrasound combined with microbubbles, Proceedings of the National Academy of Sciences (2023). DOI: 10.1073/pnas.2212933120
Journal information:
Proceedings of the National Academy of Sciences
Source: Read Full Article