Miami Cancer Institute, part of Baptist Health South Florida, announced the publication of a multi-institutional retrospective cohort study about the impact of immune checkpoint inhibition (ICI) and single-fraction stereotactic radiosurgery (SRS) on radiation necrosis (RN) in patients with brain metastasis from non-small cell lung cancer.
The study, titled “Immune Checkpoint Inhibition and Single Fraction Stereotactic Radiosurgery in Brain Metastases from Non-Small Cell Lung Cancer: An International Multicenter Study of 395 Patients” is published in the Journal of Neuro-Oncology.
“One of the key findings of the study is that immune checkpoint inhibition, when administered together with stereotactic radiosurgery, does not increase the risk of radiation necrosis,” said Manmeet S. Ahluwalia, M.D., MBA, FASCO, chief of medical oncology, chief scientific officer, deputy director, and Fernandez Family Foundation Endowed Chair in Cancer Research at Miami Cancer Institute, and senior author of the study. “We did, however, find a relationship between the volume of the brain area that is targeted during radiation and radiation necrosis.”
The study included 395 patients with 2,540 brain metastases who were treated with SRS and ICI across four countries with a median follow-up of 14.2 months. The median age of the study participants was 67 years. The median margin SRS dose was 19 Gy, but 36.5% of patients had a V12 Gy of larger or equal to 10 cm3.
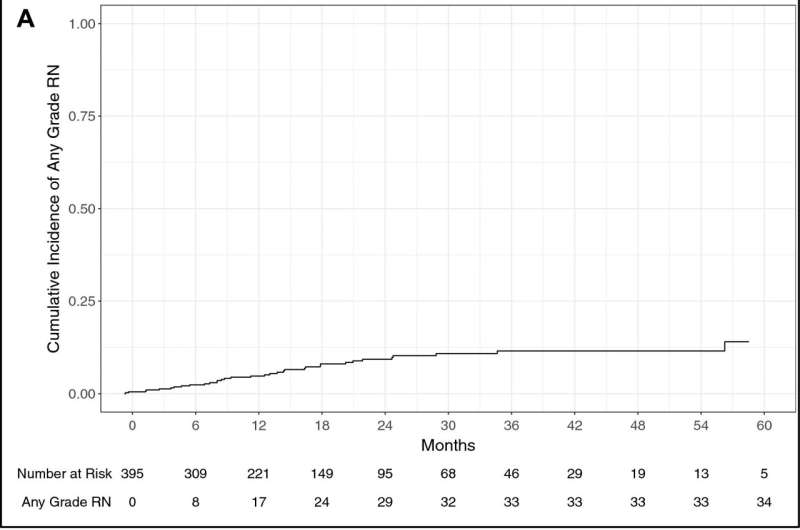
On multivariable analysis, V12 Gy of larger or equal to 10 cm3 was a significant predictor of developing any grade RN and symptomatic RN (SRN). At one year, the cumulative incidence of any grade RN and SRN for all patients was 4.8% and 3.8%, respectively. For concurrent and non-concurrent groups, the cumulative incidence of any grade RN was 3.8% versus 5.3%, respectively; and for SRN was 3.8% vs. 3.6%, respectively.
“The risk of any grade radiation necrosis and symptomatic radiation necrosis following single fraction stereotactic radiosurgery and immune checkpoint inhibition for non-small cell lung cancer brain metastases increases as V12 Gy exceeds 10 cm3,” added Ahluwalia.
“Concurrent immune checkpoint inhibition and stereotactic radiosurgery do not appear to increase this risk. Instead, radiosurgical planning techniques should aim to minimize V12 Gy. In addition, the study suggests that treatment with immune checkpoint inhibitors can continue when radiation necrosis occurs.”
More information:
Eric J. Lehrer et al, Immune checkpoint inhibition and single fraction stereotactic radiosurgery in brain metastases from non-small cell lung cancer: an international multicenter study of 395 patients, Journal of Neuro-Oncology (2023). DOI: 10.1007/s11060-023-04413-4
Journal information:
Journal of Neuro-oncology
Source: Read Full Article