 insights from industryDr. Shebna MasseyAssociate Product ManagerSino Biological US Inc.
insights from industryDr. Shebna MasseyAssociate Product ManagerSino Biological US Inc.In this interview, Dr. Shebna Massey discusses neurodegenerative diseases such as Alzheimer's, Parkinson's, Huntington's, and more. She also discusses and explores new therapeutic targets and biomarkers for these diseases.
How much is known about the etiology and pathogenesis of neurodegenerative diseases?
Increasing life expectancy has led to silently progressive neurodegenerative disorders becoming more prominent worldwide.
The combined effects of genetic aberrations, environmental factors, and age are mainly attributed to the onset of neurodegenerative disorders like Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), and Amyotrophic lateral sclerosis (ALS).
The progressive loss of neurons, the dysfunction of glial cells, and disruption in synaptic connections in the brain and spinal cord pathologically characterize these disorders.
Some new paradigm-shifting etiological views propose that cardiovascular diseases are the basis of homeostatic disruptions of various proteins affecting cognitive functioning.
There are also studies highlighting the immunomodulatory functions of the gut-brain axis. An integrated and innovative approach is required to incorporate these views into the traditional and classical etiological views and research of neurodegenerative disorders.
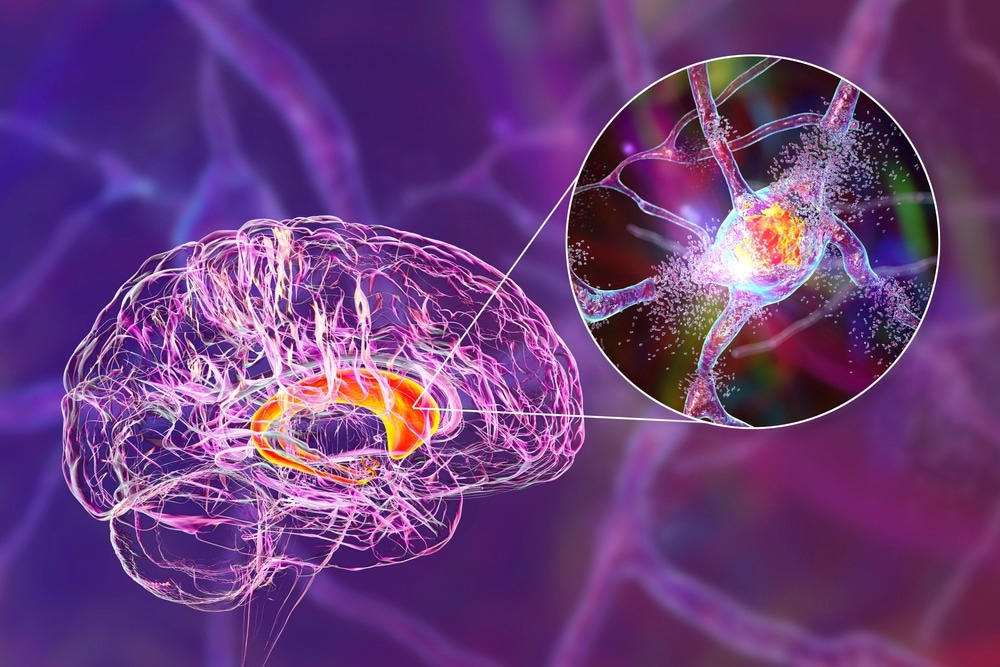
Image credit: Kateryna Kon/Shutterstock.com
What are the common therapeutic targets in neurodegenerative disorders? What stages of development are they at?
Neurodegenerative disorders are identified based on the association of abnormally conformed toxic proteins, such as tauopathies, α-synucleinopathies, TDP-43 proteinopathies, and FUS/FET proteinopathies, where the associated proteins are Tau, a-synuclein, TDP-43, and FUS/FET, respectively.
The aggregation of these abnormal proteins leads to the formation of tangles and plaques that cause neurodegeneration. One of the most popular proteins associated with neurodegenerative disorders is amyloid-beta, frequently detected as a co-accumulative protein with Tau in Alzheimer’s disease.
Amyloid and Tau proteins have been established through investigation as therapeutic targets. Immunotherapy is the most advanced approach in the drug development stage for most of these targets, but vaccines and humanized antibodies also target disease-associated proteins.
Experimental Alzheimer’s drugs targeting the Tau protein have entered clinical trials this year. They will be studied under the Dominantly Inherited Alzheimer Network Trials Unit (DIAN-TU) trials for the next decade. A promising antibody, gantenerumab, which targets amyloid, was also successful in a Phase 2/3 clinical trial under the same program.
Amyloid plaques are associated with several neurodegenerative diseases, meaning that successful treatments provide hope that similar conditions may be cured.
Video credit: Sino Biological Inc.
Many drugs that target amyloid-β (Aβ) in Alzheimer's disease (AD) have failed to demonstrate clinical efficacy. Does this indicate the need for the discovery of novel targets? What is the current progress for this?
Amyloid plaques were first reported in the 1800s in patients with dementia. Since then, the amyloid-β (Aβ) protein that promotes the formation of these plaques has been studied and observed as a critical step in pathogenesis in many neurodegenerative disorders, particularly AD.
However, most treatments targeting Aβ have not been clinically successful. This has sparked the idea that these aggregation events might be preceded and, more importantly, dominated by other significant events that regulate this protein.
A recent study published in Nature Neuroscience has challenged the conventionally accepted sequence of events leading to plaque formation, where Aβ is thought to initiate the domino effect of neurodegeneration.
This study has instead linked autophagy dysfunction to the formation of amyloid plaques with strong in vivo evidence from five different mouse models. This will require further investigation to identify a pivotal target to validate and extend into clinical studies.
Co-aggregation with Aβ also makes Tau a preferred therapeutic target. Clinical trials on Tau as the target of antibodies or radiotracers in positron emission tomography (PET) make it a strong alternate candidate. Among all the clinical trials targeted toward AD, 40% are centered on Aβ and 18% on Tau.
Some small molecule inhibitors are being tested for targets in neuroprotection, neuroinflammation, growth factors, and neurometabolic and cardiovascular pathways, including molecules like IL-6, IFNGR1, p75NTR, APOE, GSK3β, ADRA2B, and CSF factors.
What models, tools, and research strategies are used for drug target discovery in neurodegenerative diseases?
The traditional approaches to drug discovery compared affected individuals with control groups to identify symptomatic, physiological, and genetic differences to identify the disease states.
New methods focus on genetically and anatomically evaluating vulnerable and resistant neuron populations from the same individual to find physiological and genetic uniqueness that makes one region disease-prone and the other protected from pathogenesis.
The current studies are more comprehensive; instead of studying only one disease stage, they are designed to recapitulate pre-disease and post-disease initiation stages and disease progression.
More high-throughput approaches are employed, involving total gene expression analysis and genome-scale RNA profiling.
In silico models and experimental strategies are being utilized for drug target discovery to save the time and cost of experimentation on large data sets generated by next-generation sequencing and large-scale neuroimaging profiling.
They are combined with molecular docking to predict molecular conformation and optimize drug-target interactions of large libraries of compounds before transferring and testing various molecule-drug combinations in vivo.
These strategies are expected to fill the large gap between the design, production, and testing of efficacious drugs for neurodegenerative diseases.
What progress is there in biomarkers and the monitoring of neurodegenerative diseases?
Early diagnosis is critical for providing well-designed and suitable treatment plans to prevent disease progression. The current biomarkers in neurodegenerative diseases are mainly amyloid-β plaques and Tau tangles, detected in magnetic resonance imaging (MRI) and positron emission tomography (PET).

Image credit: Chinnapong/Shutterstock.com
These markers have effectively improved the diagnostic and treatment outcomes of Alzheimer’s disease. However, the most promising biomarkers, like TREM2, a-synuclein, and SV2A, have failed to display adequate specificity and sensitivity in clinical testing and are still under investigation.
Ubiquitin levels are also proposed as biomarkers to monitor disease progression, along with neurofilament light, FYN, and BACE1.
During the pandemic, some significant advances were made in establishing blood-based biomarkers. These blood tests can detect an AD-specific phosphorylated form of Tau in blood.
These biomarkers are detectable early in the disease, meaning that they have the potential to be good diagnostics and prevent disease progression.
What does the future look like in terms of the discovery and implementation of novel biomarkers in neurodegenerative diseases?
Recently, there has been a steady increase in the examination of neuroinflammatory and neurovascular molecules as potential biomarkers. Some proposed biomarkers and drug targets are TREM2, GFAP, MCP-1, MAPK1, VEGFR1, and FGFR1.
Targeting these molecules is predicted to reduce neuroinflammation, improve blood-brain barrier functions, and prevent neurodegeneration.
With an increasing understanding of the pathogenesis of neurodegenerative diseases, there is a shift in the treatment strategy toward enhancing the neuroprotective mechanisms of the cells. Growth factors like BDNF, NGF, and GDNF help neurons to survive, maintain and regenerate, making them potential therapies for neurodegenerative illnesses.
Clinical studies for GDNF (a treatment for Parkinson’s disease), NGF (a cure for Alzheimer’s disease), and BDNF (a treatment for both AD and PD) are underway. Additionally, when it comes to neuroimaging and the treatment of neurodegenerative disorders, non-invasive cell-state-specific novel PET ligands have huge potential.
Sino Biological is helping scientists to drive neurodegenerative disorders research by providing quality recombinant proteins, antibodies, ELISA kits, gene products, and CRO services.
About Dr. Massey
Dr. Massey received her undergraduate degree from the University of Houston-Downtown and her Ph.D. in Integrative Molecular and Biomedical Sciences from the Baylor College of Medicine. Her dissertational work focused on establishing a drug-targetable post-transcriptional regulatory program in breast cancer metastasis. She is currently working as an Associate Product Manager at the Sino Biological US Inc., Houston. She is interested in scientific advances in drug discovery and cancer immunotherapy.
About Sino Biological Inc.

Sino Biological is an international reagent supplier and service provider. The company specializes in recombinant protein production and antibody development. All of Sino Biological's products are independently developed and produced, including recombinant proteins, antibodies and cDNA clones. Sino Biological is the researchers' one-stop technical services shop for the advanced technology platforms they need to make advancements. In addition, Sino Biological offers pharmaceutical companies and biotechnology firms pre-clinical production technology services for hundreds of monoclonal antibody drug candidates.
Sino Biological's core business
Sino Biological is committed to providing high-quality recombinant protein and antibody reagents and to being a one-stop technical services shop for life science researchers around the world. All of our products are independently developed and produced. In addition, we offer pharmaceutical companies and biotechnology firms pre-clinical production technology services for hundreds of monoclonal antibody drug candidates. Our product quality control indicators meet rigorous requirements for clinical use samples. It takes only a few weeks for us to produce 1 to 30 grams of purified monoclonal antibody from gene sequencing.
Sponsored Content Policy: News-Medical.net publishes articles and related content that may be derived from sources where we have existing commercial relationships, provided such content adds value to the core editorial ethos of News-Medical.Net which is to educate and inform site visitors interested in medical research, science, medical devices and treatments.