Menopause, the end of menstrual cycles, can produce symptoms such as hot flashes, night sweats, insomnia and mood changes. Women do not need to suffer in silence: Many treatment options are available. Jewel Kling, M.D., chair of the Division of Women’s Health at Mayo Clinic in Scottsdale, Arizona, describes hormonal and nonhormonal therapies.
“We sometimes hear the question, ‘Do I need to treat hot flashes or night sweats?’ and the answer for many may be, ‘Yes,'” Dr. Kling says. “Because hot flashes and night sweats affect quality of life and productivity at work and at home for women.”
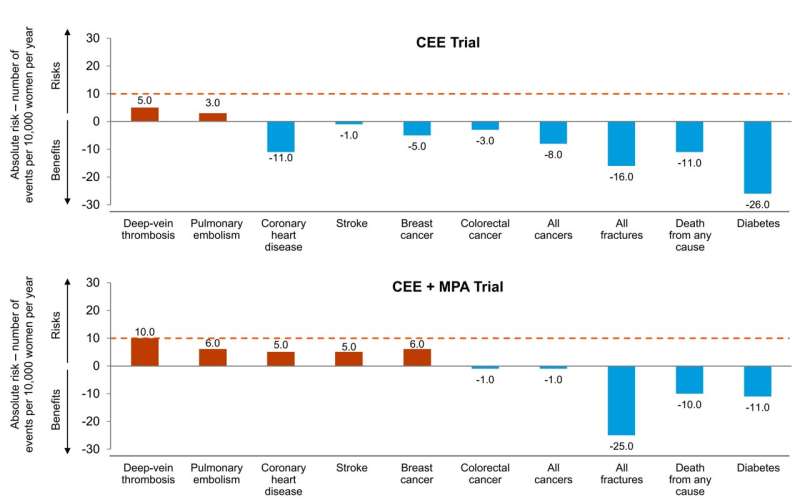
Hormone replacement therapy is an estrogen medication; for women with a uterus, hormone therapy typically includes estrogen plus progestogen medication to prevent endometrial cancer. For women younger than 60 or within 10 years after their final period, the benefit of hormone therapy outweighs the risk in healthy women with postmenopausal symptoms, according to recent guidelines from the North American Menopause Society published in Menopause.
“Many factors affect a woman’s decision whether to use hormones and if she uses them, which particular regimen is best to relieve her symptoms,” Dr. Kling says. “Common factors considered include age, underlying health, symptom severity, preferences, available treatment options, and of course, cost considerations. One important consideration is whether the potential benefits outweigh the potential risks.”
Among benefits
Many studies have shown that systemic hormone therapy such as a pill, patch, gel or spray, helps with hot flashes, night sweats, and vulva vaginal symptoms, Dr. Kling says.
There’s also strong evidence that long-term treatment with estrogen therapy or estrogen plus progestogen therapy reduce the risk of fractures after menopause.
“Along with these benefits often comes improvement with menopause-related symptoms, including those most likely bothersome, including disturbed sleep, mood problems, and diminished sexual satisfaction,” Dr. Kling says. “Addressing these symptoms can lead to a better quality of life.”
Among risks
With oral systemic estrogen therapy or estrogen plus progestogen therapy, risks include blood clots in the legs and lungs, and stroke.
“Stroke is dependent on the age at which a woman starts hormone therapy. Specifically, the risks are low for women younger than 60 or within 10 years after their last period,” Dr. Kling says. “There do not appear to be the same risks associated with transdermal estrogen products such as patches, particularly when we use lower doses.”
- Use of estrogen alone by women who have a uterus carries a risk of uterine cancer; that risk can be lowered by including progestogen or an estrogen selective estrogen receptor modulator, also known as the SERM (selective estrogen receptor modulator) combination.
- Breast cancer risks should also be considered, and appear slightly higher, particularly in women with a uterus who use estrogen plus a progestogen.
“However, overall, the risk of serious events with hormone therapy are rare,” Dr. Kling says. “For women with only vaginal symptoms, low-dose vaginal estrogen can be used. Low-dose vaginal estrogen does not have the same risks as systemic therapy because the body absorbs very little.”
Hormone therapy generally isn’t an option for women with breast cancer, other hormonally mediated cancers or blood clot issues, and other women may simply wish to avoid hormone therapy, Dr. Kling says. There are many nonhormonal therapies ranging from mind-body techniques to medication that can bring relief with few or no side effects:
- There is some evidence that losing weight may reduce hot flashes and night sweats.
- Among medications, low-dose paroxetine has been shown to help some women with symptoms such as hot flashes. At low doses, it doesn’t appear to cause weight gain or have adverse sexual effects.
- In some cases, antidepressants may be appropriate, and the health care practitioner and patient will weigh benefits and risks, Dr. Kling says.
- Mind-body techniques include cognitive behavioral therapy and clinical hypnosis, both of which depend on expert guidance for success, Dr. Kling says. Some patients have found relief from acupuncture, yoga and meditation.
“There are many ways to help women deal with the discomfort and diminished quality of life associated with menopause,” Dr. Kling says. “Women don’t need to simply tough it out. They can get help.”
More information:
The 2022 hormone therapy position statement of The North American Menopause Society, Menopause (2022). DOI: 10.1097/GME.0000000000002028
Journal information:
Menopause
Source: Read Full Article