Myelin is an insulating sheath around axons—the processes connecting nerve cells—that is mostly composed of lipids and proteins. It enables rapid conduction of electrical signals and supports neuronal integrity and function. In the central nervous system, myelin is formed by specialized glial cells called oligodendrocytes.
Myelinated fiber tracts are particularly vulnerable to various pathogenic processes and myelin diseases are often associated with chronic inflammation of the nervous system. A prime example is multiple sclerosis, a serious and frequent neurological disease in which immune cells drive demyelination, i.e., the loss of myelin. However, maladaptive immune reactions also contribute to other disorders associated with myelin defects, including hereditary and aging-related diseases.
Importantly, the degeneration of axons and neurons is a major determinant of clinical disease severity in such disorders. It is generally assumed that loss of myelin leads to increased vulnerability of denuded axons to a toxic inflammatory milieu and ultimately results in their demise.
This purely detrimental view of demyelination is challenged by a recent study conducted at the Department of Neurology under corresponding author and lecturer Dr. Janos Groh from the Section of Developmental Neurobiology (Prof. Dr. Rudolf Martini, University Hospital Würzburg) and in collaboration with the Institute of Molecular Neurobiology (Prof. Dr. Mikael Simons, Technical University of Munich).
Supported by Prof. Dr. Antoine-Emmanuel Saliba from the Helmholtz Institute for RNA-based Infection Research (Würzburg) and teams of researchers from Hannover, and Cambridge, they have now published the results of their study in the journal Nature Communications.
Myelin gene defects instigate distinct immune reactions
To investigate the relationship between loss of myelin and axon degeneration, the researchers studied mouse models of rare diseases carrying defects in the major myelin protein of the central nervous system. “These models of rare monogenetic diseases offer unique opportunities to reveal mechanisms that have broad relevance for much more frequent disorders,” says Rudolf Martini.
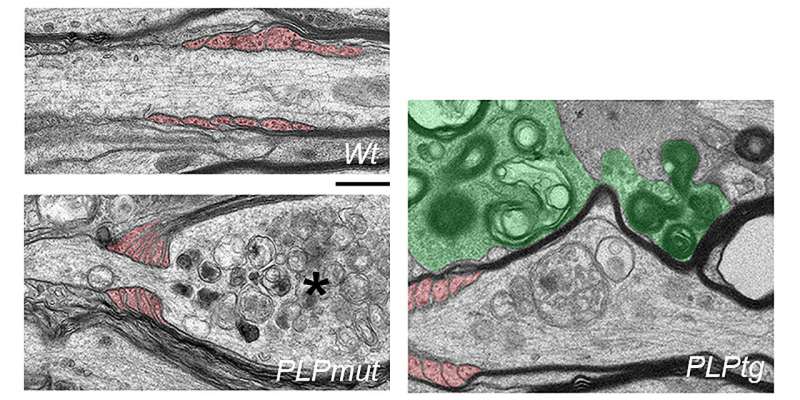
The scientists had previously discovered that the formation of abnormal or “bad” myelin in these mice leads to an inflammatory reaction comprising an accumulation of cytotoxic CD8+ T cells. In the analyzed disease models, these adaptive immune cells target and damage fiber segments with abnormal myelin, reminiscent of multiple sclerosis.
Surprisingly and in contrast to the prevailing view, they found an inverse relationship of axon loss and demyelination when comparing the disease models. Fibers that remained myelinated despite the chronic attack of T cells had a higher risk to degenerate, while those that lost their myelin survived. Moreover, behavioral deficits of the mice correlated more clearly with neurodegeneration than demyelination.
Persistence of abnormal myelin as a risk factor for axon degeneration
“This inverse relationship was unexpected and prompted us to study the interactions of abnormal oligodendrocytes and another immune cell type called microglia in more detail,” explains Janos Groh. Microglia are cells of the innate immune system that populate the central nervous system and can orchestrate detrimental as well as beneficial immune reactions.
In their study, the authors used different pharmacological approaches to modulate the removal of abnormal myelin by microglia. “We show that efficient microglia-mediated removal of perturbed myelin under adaptive immune attack allows the survival of axons at reversible stages of damage,” Groh adds. Thus, persistent ensheathment with “bad” myelin seems to be worse for neurons than the loss of myelin, at least when myelin is targeted by adaptive immunity.
Oligodendrocytes under immune attack actively harm axons
The scientists could also identify a mechanism for how oligodendrocytes attacked by T cells harm their axonal partners. They found an aberrant constriction response at the myelinating processes wrapped around the axons. “When we inhibited this aberrant constriction by paralyzing cytoskeletal filaments, we could reduce axon degeneration,” Groh says.
“The T cell attack seemed to incite oligodendrocytes to strangulate axons like a constrictor snake,” Martini adds.
“What is the biological sense of these highly organized, but self-mutilating processes?” Martini says. The researchers speculate that these reactions of oligodendrocytes can be beneficial in other conditions, like injuries to the nervous system. However, aberrant induction of these immune-driven mechanisms might be a harmful response in many diseases.
According to Groh and Martini, their study identified putative targets for therapy in diseases associated with myelin defects and inflammation in the nervous system. Moreover, they emphasize that novel therapeutic approaches for myelin diseases ideally should block detrimental but still allow beneficial immune responses, like the removal of “bad” myelin. This might help to foster neural resilience mechanisms as a prerequisite for recovery from damage to the nervous system.
More information:
Janos Groh et al, Microglia-mediated demyelination protects against CD8+ T cell-driven axon degeneration in mice carrying PLP defects, Nature Communications (2023). DOI: 10.1038/s41467-023-42570-2
Journal information:
Nature Communications
Source: Read Full Article