The glymphatic system is the brain’s self-cleaning mechanism. If you haven’t heard of the glymphatic system, it’s probably because it wasn’t discovered until 2012. Since then, there’s been a surge of research investigating the role of glymphatic system dysfunction in various brain pathologies.
The glymphatic system is intimately tied to the circadian system and sleep architecture, and both are implicated in the pathophysiology of concussions. Here, I’ll explain the glymphatic system’s nature, how its dysfunction contributes to concussion pathology, and the crucial role of circadian therapy in mitigating this impact.
Our review on the topic is also published in the journal Science Progress.
The garbage truck of the brain
The glymphatic system, derived from the term “glial-lymphatic system,” was nicknamed “the garbage truck of the brain” by its discoverer, Maiken Nedergaard.
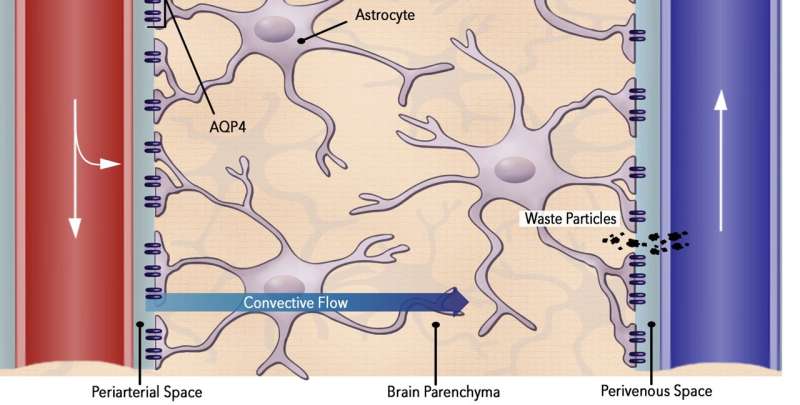
Its fundamental role is to remove waste products from the brain. This is achieved through the convective flow of cerebrospinal fluid (CSF) from arterioles to venules, facilitated by water channels called aquaporins (AQP-4, in particular).
How the glymphatic and circadian systems are related
Approximately 80–90% of glymphatic clearance occurs during “deep sleep.” This stage of sleep is characterized by synchronized brainwaves, a feature that facilitates the influx of CSF into the brain’s interstitial space.
As sleep transitions from deep sleep into the more tumultuous signals of REM sleep, the fluid is effectively flushed out. Thus, the rhythmic oscillation between deep sleep and REM parallels the “rinse-and-repeat” cycle of the glymphatic system. It’s fascinating that the neurophysiological purpose of the dream cycle is to purge physical waste from the brain!
Thus, a bidirectional relationship exists between the optimal operation of the glymphatic system and sleep architecture, which itself is governed by circadian oscillators.
When this equilibrium is disturbed, both systems become disordered and neurotoxic waste builds up in the brain, leading to the manifestation of neurological symptoms. This dynamic is evident in diverse clinical contexts, including sleep-deprivation psychosis, advanced-stage dementia, the “brain fog” of sleep apnea, and concussion pathophysiology. Indeed, some researchers have proposed the term “CNS interstitial fluidopathies” for this group of conditions.
Concussions disrupt both the glymphatic and circadian systems
In concussions, we see a substantial decline in glymphatic system functioning. In experimental models, this decline in function approaches 60%. Concurrently, there’s a significant drop in melatonin levels in both CSF and saliva, causing circadian system dysfunction.
This dual hit to the glymphatic and circadian systems subsequently drives the widespread occurrence of sleep disturbances following concussions. Thus, a vicious cycle is created between glymphatic dysfunction and sleep disruption.
Not surprisingly, patients with prolonged sleep dysfunction are at an increased risk of persistent post-concussion symptoms (i.e., post-concussion syndrome). The putative explanation for this is that with impaired glymphatic clearance, neuroinflammation persists in the acute phase, setting the stage for central sensitization and chronic neurologic symptoms, such as post-traumatic headaches and photophobia
The special case of chronic traumatic encephalopathy
Chronic traumatic encephalopathy (CTE) is the tragic disease that affects people who’ve had repeated concussion injuries. The histological hallmark of CTE is progressive perivascular tau deposition. The glymphatic system allows us to better understand this, as each concussion leads to an increase in perivascular tau burden and greater glymphatic system dysfunction.
To better explain this, picture capillaries in the brain as storm drains, concussions as storms, and tau proteins as leaves. Under normal circumstances, the leaves can easily flow into the storm drain. However, when a storm occurs, the sheer volume of leaves overwhelms the storm drain’s capacity to clear them. With each subsequent storm, there’s an increasing incapacitation of the drain’s ability to clear away the leaves. This is precisely what happens with the progressive perivascular tau deposition in CTE.
This reveals the importance of implementing circadian therapy after each concussion. By optimizing sleep architecture, circadian therapy has the potential to mitigate glymphatic dysfunction, thereby augmenting the clearance of neurotoxic proteins like tau. To use the analogy above, circadian therapy is like using a hose to help clear the leaves from the storm drain after a storm.

Circadian therapy rescues the glymphatic system after concussions
We have the potential to enhance glymphatic function through circadian therapy interventions. The clinical significance of this is two-fold. First, when used in the acute setting, improved glymphatic clearance can decrease neuroinflammation and reduce the risk of central sensitization and persistent post-concussion symptoms. Second, augmenting glymphatic clearance of tau proteins potentially decreases the risk of future CTE development, essentially “de-risking” the concussion.
Some specific examples of circadian therapy tools include:
- Melatonin supplementation
- Screen time restriction
- Evening light restriction
- Morning blue light therapy
- Sleep hygiene measures
- Sleep apnea screening and treatment
- Omega oil supplementation (for its effect on AQP-4 channels)
- Sleep cognitive behavioral therapy
- Prescribed exercise
Each of these interventions have individually demonstrated its effectiveness in enhancing sleep, and several specifically improve concussion outcomes. Circadian therapy in this context is the programmatic implementation of these measures, with the goal of augmenting glymphatic system clearance.
Moving from reactive to proactive concussion care
Currently, the paradigm is shifting in terms of how clinicians manage concussions, from reactive to proactive care. Circadian therapy fits well in this new proactive care model and these tools should be implemented early in the recovery process, when glymphatic dysfunction is the worst.
The rationale for incorporating circadian therapy into acute concussion management is strong, considering the pervasive sleep disturbances following concussions and the significance of compromised sleep on glymphatic function. We’re implementing these measures in our concussion clinic and look forward to seeing this approach grow in the community of concussion providers.
This story is part of Science X Dialog, where researchers can report findings from their published research articles. Visit this page for information about ScienceX Dialog and how to participate.
More information:
Sohaib Kureshi et al, Circadian therapy interventions for glymphatic dysfunction in concussions injuries: A narrative review, Science Progress (2023). DOI: 10.1177/00368504231189536
Sohaib Kureshi, MD, is a board-certified neurosurgeon who practices out of San Diego. Dr. Kureshi earned his medical degree from the University of Southern California (USC) School of Medicine and completed internship and neurosurgical residency at Duke University. Dr. Kureshi is an expert in the treatment of traumatic brain injuries and is the CEO and Founder of TBI Virtual, a telehealth clinic that specializes in concussion management. He is a member of the American Association of Neurological Surgeons, the Congress of Neurological Surgeons, and the San Diego Medical Society.
Source: Read Full Article