Beyond traditional models: 3D bioprinted tumor microenvironment unlocks resistance insights
In a recent study published in Scientific Reports, researchers developed a three-dimensional (3D) biologically printed in vitro model of the breast cancer tumor microenvironment (TME) consisting of simultaneously cultured cells dispersed in hydrogels with a controlled design to assess tumor heterogeneity.
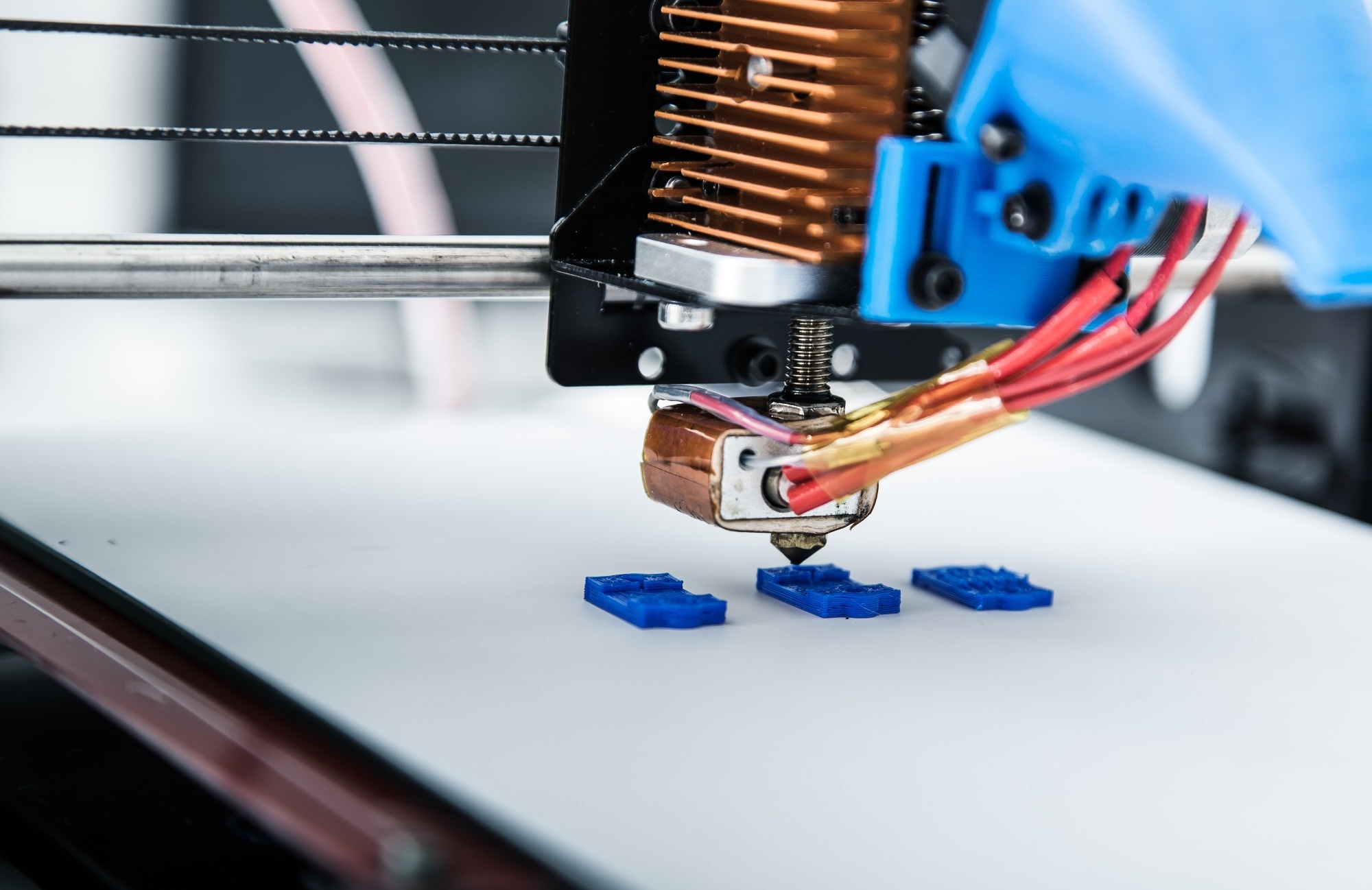 Study: Controlled tumor heterogeneity in a co-culture system by 3D bio-printed tumor-on-chip model. Image Credit: Alex_Traksel/Shutterstock.com
Study: Controlled tumor heterogeneity in a co-culture system by 3D bio-printed tumor-on-chip model. Image Credit: Alex_Traksel/Shutterstock.com
Background
Breast cancer is the most common cancer in women and the second most common overall. Tumor heterogeneity contributes to its aggressiveness, with intercellular and cell-tumor microenvironment interactions playing a crucial role in tumor invasion and advancement.
Limited studies have utilized organ-on-a-chip platforms to study heterogeneity in breast cancer. An effective model must cover tumor heterogeneity to accurately study cancer progression.
About the study
In the present study, researchers developed a platform using 3D biological printing to model the phenotypic heterogeneity resulting from different cell localizations in a tumor.
The researchers created a framework for modelling the phenotypic heterogeneity that can emerge in cancer as a result of varied cell localization (tumor centre or periphery, unequal oxygen amount) and/or interaction with the tumor microenvironment (TME).
Triple-negative breast tumor cells with mesenchymal features (MDAMB231), breast adenocarcinoma cell line (MCF7), and non-cancerogenic mammary epithelial-type (MCF10A) cells were implanted in gelatine-alginate hydrogels for printing by a multiple-cartridge extrusion-type biological printer to create cellularly heterogeneous samples with the two different breast cancer cells in particular initial locations, specific architecture, and controlled density.
The breast cancer cells were encapsulated in hydrogels before being printed using an extrusion-based bioprinter to construct a 3D model tumor to imitate the in vivo microenvironment. All hydrogels exhibited shear-thinning behaviour, and A4G4 was chosen as the optimal hydrogel for co-culture tests based on printability and viability results.
To induce cellular heterogeneity, the team mixed the cells randomly or arranged them in consecutive layers. A progressive chemical gradient was created to analyze cell migration in the direction of the epithelial growth factor (EGF) chemoattractant in MCF10A cell presence in varied ratios.
Printability and cell viability studies were used to refine the bioink. Individual pressure and speed controls controlled the material flow for each print head. The printability of alginate-gelatin hydrogels was investigated using a combination of various hydrogel compositions and printing pressures.
Cell viability was assessed on the printed structures immediately after bioprinting as well as four, seven, and eleven days later using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) and live and dead assays.
Laser scanning confocal microscopy was used to investigate the construct. The elastic and viscous moduli of the hydrogels were evaluated using rheological tests of bioink compositions.
A tree-like gradient generator was created that could be combined with the tumor-on-chip model's three-dimensional biological printing. The model had a length of 45 mm and a width of 21 mm. The microfluidic gradient generator was built using standard lithography techniques.
Results
The method enabled fine control over the position and arrangement of cells in a coculture system, allowing the creation of diverse tumor designs. Bioprinting was continued using a 22G nozzle, which requires less extrusion pressure and was shown to be beneficial to cell survival after printing.
According to the results of the live-dead cell assay, the proportion of live MDA-MB-231 breast cancer cells immediately after bioprinting was 94%, 85%, 97%, and 76%, and for the A1G4, A1G8, A4G4, and A8G4 hydrogels, respectively.
The interlinked porous structure of the hydrogel constructions guaranteed nutrition diffusion inside the construct provided an adequate environment for live cells, and permitted the diffusion of waste products from the construct.
The team observed excellent cell dispersion inside the construct with an absorbance value of 0.9 immediately after printing.
Absorbance climbed to 1.4 in four days and 1.9 in a week. The survivability rate rose during the week as compared to the first day; however, an absorbance value of 2.1 was observed on day 11, indicating a decrease in the cell proliferation rate.
Between days 7.0 and 11, the constructions achieved their maximal capacity for cellular hosting, and a few cells died as a result. The findings indicated that 3D biologically printed hydrogel constructions are biocompatible and can keep cells alive for a long period of time.
The initial biologically printed structural layer comprised MDA-MB-231 breast cancer cells, while the subsequent layer comprised MCF7 breast tumor cells and was placed above the initial layer.
The cell population and cell ratio were different near the margins of the 2D chamber compared to the centre of the chamber, but the tumor cells were placed uniformly in the 3D biologically printed structure.
Imaging of the co-cultured three-dimensionally printed constructs showed both breast cancer cell types were present in all layers randomly since they were printed on day one and after three days, the cells formed clusters.
MCF7 cells appeared to be more prone to migrating to MDA-MB-231 since more numerous mixed cell type clusters were identified than MCF7 cell clusters.
MDA-MB-231 breast cancer cells migrated more quickly toward the EGF chemoattractant than MCF7 cells. When the ratio of cancer cells to non-cancerous cells was 1:1, the migratory propensity was greatest.
Because of the high extrusion pressure, which imposes more shear stress on cells, very viscous hydrogels result in reduced cell viability.
The MTT results showed that the rate of viability rose during the week compared to day one, confirming the cells' accessibility to nutrients and oxygen.
Conclusion
Overall, the study findings showed a strategy using the convergence of 3D bioprinting and microfluidic devices to produce distinct tumor structures typical of those observed in different individuals.
The tumor-on-chip model may help to understand cancer cell activity in heterogeneous tumors and their microenvironment with the high temporal and geographical resolution, and it may give important information for predicting the timing of metastasis in the future.
-
Moghimi, N. et al. (2023) "Controlled tumor heterogeneity in a co-culture system by 3D bio-printed tumor-on-chip model", Scientific Reports, 13(1). doi: 10.1038/s41598-023-40680-x. https://www.nature.com/articles/s41598-023-40680-x
Posted in: Device / Technology News | Medical Procedure News | Medical Science News | Medical Research News | Medical Condition News | Women's Health News
Tags: Adenocarcinoma, Assay, Bioprinting, Breast Cancer, Cancer, Cell, Cell Line, Cell Migration, Cell Proliferation, CHIP, Confocal microscopy, Growth Factor, Hydrogel, Imaging, in vitro, in vivo, Lithography, Metastasis, Microscopy, Nutrients, Nutrition, Oxygen, Proliferation, Stress, Tumor

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.