Prof. Yossi Buganim and his research team at the Faculty of Medicine at the Hebrew University of Jerusalem have achieved a groundbreaking milestone in the field of cell reprogramming. Their latest study, published in Nature Communications, reveals a remarkable breakthrough in converting skin samples into functional human placenta cells. This achievement has significant implications for understanding pregnancy development, studying pregnancy-related diseases, and advancing cell therapies.
The research opens new avenues for investigating the causes of infertility, complications during pregnancy, and long-term health implications for both mothers and babies.
Reprogramming cells to assume new identities has been a focus of Prof. Buganim’s lab, which utilizes specialized proteins to modify gene expression. By transforming skin cells into other cell types, the team enables the study of specific diseases and the potential development of cell-based therapies. However, accessing cells from the placenta, a critical organ in pregnancy, has long been a challenge due to technical and ethical constraints.
The recent research from Prof. Buganim’s lab overcomes these hurdles by deriving early placental cells from skin samples. This breakthrough provides an unlimited supply of cells for studying placental function. Moreover, individuals who experienced complicated pregnancies can shed light on the mechanisms behind pregnancy complications by utilizing skin-derived cells with the same genetic makeup that might have contributed to placental dysfunction.
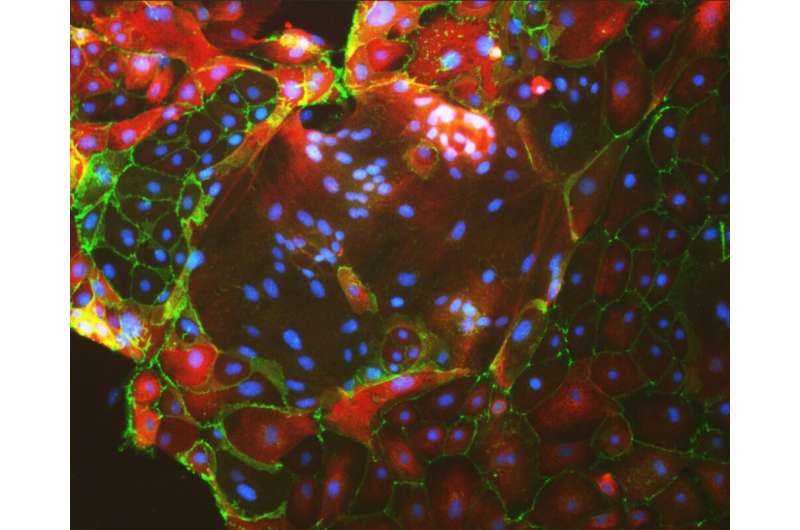
To achieve this, the team identified a set of genes governing the identity of placental stem cells (also termed trophoblast stem cells—TSCs), the precursor cells responsible for placental development. By inducing the expression of these genes in skin cells, the researchers successfully converted the skin cells, into functional and stable placental stem cells. These induced placental stem cells exhibited similar properties to cells obtained from early pregnancies and possessed the ability to give rise to different placental cell subtypes. Comprehensive analyses, including multi-omics comparisons, validated the superiority of this method over previously published approaches.
The project was led by Dr. Moriyah Naama, an MD/Ph.D. program participant at Hebrew University, in collaboration with Ms. Moran Rahamim, a Ph.D. student, and other members of the Buganim lab. The scientists utilized over-the-counter pregnancy tests to quickly evaluate their reprogrammed cells, as these cells produce various pregnancy hormones, including human chorionic gonadotropin (hCG). The team received guidance from Prof. Simcha Yagel’s lab at the Hadassah Medical Organization’s Obstetrics and Gynecology Department and the Stem Cell Research Laboratory at Shaare Zedek Medical Center, led by Prof. Rachel Eiges, which provided critical samples from PGD-embryos.
The findings of this study hold significant promise for advancing our understanding of pregnancy development, infertility, and pregnancy-related diseases. They have the potential to revolutionize research on placental pathologies and genetic causes, leading to improved diagnostic tools and therapeutic interventions.
More information:
Moriyah Naama et al, Pluripotency-independent induction of human trophoblast stem cells from fibroblasts, Nature Communications (2023). DOI: 10.1038/s41467-023-39104-1
Journal information:
Nature Communications
Source: Read Full Article