A new study from the Kristina Broliden research group at the Department of Medicine in Solna, shows that women with a healthy bacterial flora in the vagina can simultaneously have disease-linked bacteria attached to the ectocervical mucosa. The study has recently been published in the journal Microbiome.
The new study, a collaboration between Gabriella Edfeldt, postdoctoral researcher, and Kristina Broliden, professor, shows for the first time that women can have healthy bacteria, such as Lactobacilli, in the vagina and at the same time have disease-linked bacteria, such as Gardnerella, attached to the tissue of the ectocervical mucosa. These disease-linked bacteria can provide a potential breeding ground for infections.
“We believe that these bacteria can be a reservoir that can flourish at different times and cause problems. These findings may be a key to why diseases like bacterial vaginosis often recur even after treatment. We also see that women with bad bacteria have signs of increased cell division and inflammation in the tissue, probably a defense to get rid of the bad bacteria. Women with Lactobacilli have signs of a stable and resilient mucosa. Interestingly, women with Gardnerella showed signs of a stable mucosa but with a lot of inflammation,” says Gabriella Edfeldt, currently working at the Department of Microbiology, Tumor and Cell Biology.
Globally, about 500 million women aged 15-49 years have an imbalance in the vagina, known as bacterial vaginosis (BV). There is currently no effective treatment and more than 50% relapse within one year. The disease increases the risk of HIV and HPV infection and affects fertility. The societal cost of treating BV is estimated at SEK 50 billion globally per year.
“Our study shows evidence that women have a bacterial reservoir in the tissue, which emphasizes the importance of finding treatments for BV that go deep and remove bacterial biofilm or tissue-bound bacteria. Our analysis of both gene and protein expression describes how the body’s biological mechanisms differ between women with different bacterial flora and this knowledge is important for understanding the interaction between humans and bacteria and for developing new treatments,” says Gabriella.
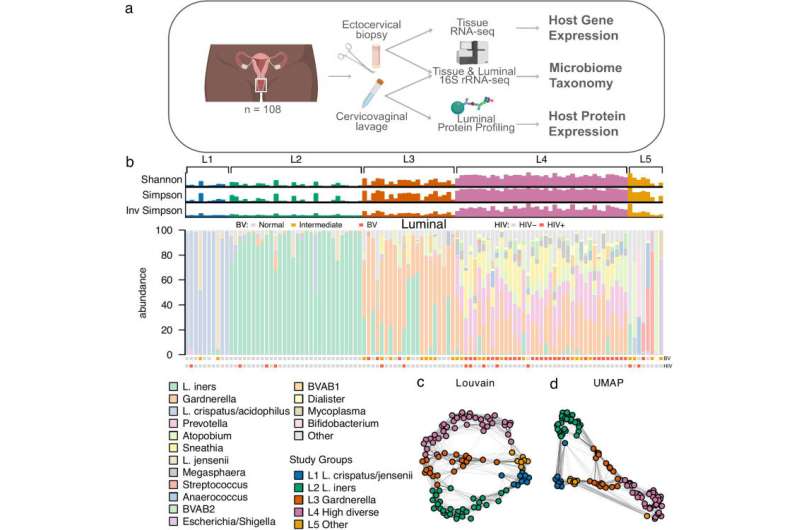
The study collected controlled biopsies and cervical swabs from 108 women aged 20-48 years, from the Pumwani Sex Worker Cohort in Nairobi Kenya, between 2013-2016. The women agreed to a 4-week work stoppage to ensure no increased risk of infection after sampling.
“The methods we used cannot tell whether the bacteria in the tissue are alive, nor describe whether they have formed a biofilm on the tissue. The study was done on a population at risk and further studies can confirm whether the results apply in other regions and populations,” says Gabriella.
“The next step in our research is to understand why some women have different bacterial flora in the tissue compared to the secretion. We will do a whole genome sequencing of the bacteria to determine if the woman has the same bacterial strains in the tissue as in the vaginal secretion, and if the bacteria in the tissue have specific genes that make them better able to stay in the tissue. We will also repeat the study in samples from the same women collected at a different point in the menstrual cycle, to confirm the results and study any differences linked to the menstrual cycle and sex hormones,” says Gabriella.
More information:
Gabriella Edfeldt et al, Distinct cervical tissue-adherent and luminal microbiome communities correlate with mucosal host gene expression and protein levels in Kenyan sex workers, Microbiome (2023). DOI: 10.1186/s40168-023-01502-4
Journal information:
Microbiome
Source: Read Full Article