Cause and mechanism
Symptoms
Genes and mutations
NADPH complex
Diagnosis and treatment
References
Further reading
Chronic granulomatous disease (CGD) is a rare genetic immunodeficiency associated with phagocyte function. It was first described in the 1950s. It is caused due to functional impairment in the NADPH (nicotinamide adenine dinucleotide phosphate) oxidase complex and affects 1 in 200,000 live births in the USA. Usually diagnosed at an early age, CGD patients are susceptible to fatal bacterial and fungal infections. Patients are treated with antibiotics and antifungal prophylaxis to prevent infections.
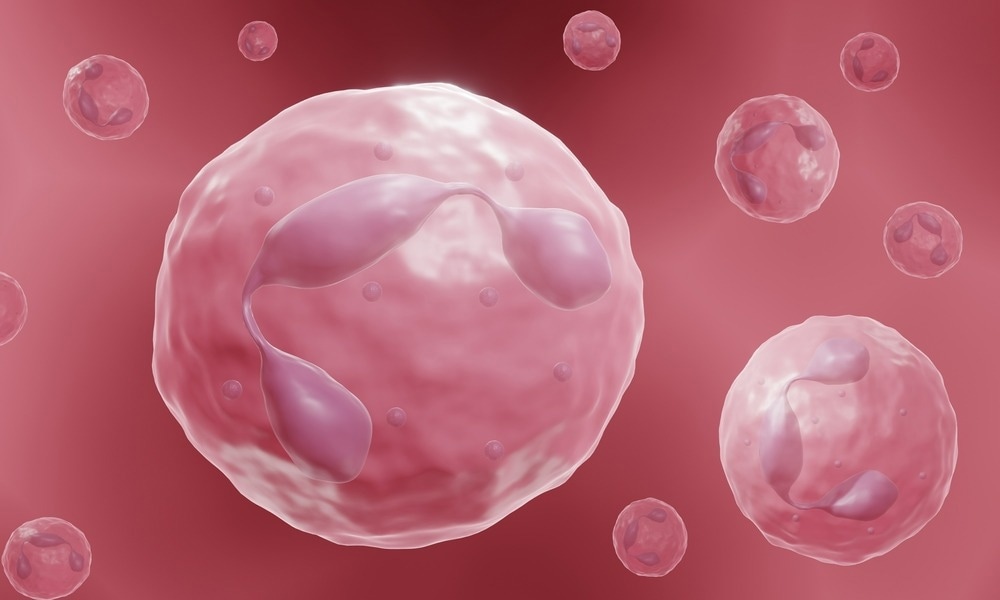
Image Credit: ART-ur/Shutterstock.com
Cause and mechanism
CGD occurs due to NADPH oxidase complex dysfunction in neutrophilic granulocytes and monocytes. It is due to mutations that inactivate NOX2 and its auxiliary proteins. These proteins work together to construct the phagocyte NADPH oxidase enzyme, which produces superoxide.
Superoxide (O2) and its reduced product hydrogen peroxide (H2O2) produce numerous reactive oxygen species (ROS) required for effective pathogen elimination. As a result, CGD patients with a dysfunctional phagocyte NADPH oxidase suffer from recurring, life-threatening infections with specific bacteria, fungi, and yeasts.
Symptoms
Clinically, CGD is highly variable, with symptoms ranging from infancy to late adulthood. The vast majority of people are diagnosed before the age of five. Children with CGD are typically short for their age.
Patients with CGD typically have bacterial and fungal infections beginning in infancy or early childhood. Staphylococcus aureus, Burkholderia cepacia species, Nocardia species, and some gram-negative enteric bacilli (Salmonella species) are common bacterial species. The lungs, skin, lymph nodes, gastrointestinal system, liver, and bones are common sites of infection. The most common causes of death are pneumonia and sepsis caused by Aspergillus or B. cepacia.
Granuloma formation is a typical consequence of CGD that can be noticed before diagnosis. Granulomatous inflammation can affect any organ system, although the gastrointestinal and genitourinary systems are the most commonly affected. A type of inflammatory bowel disease closely resembling Crohn's disease affects a significant proportion of CGD patients. The colon is usually affected; however, the ileum and other regions of the digestive tract might also be affected.
Mild diarrhea might progress to a serious condition of bloody diarrhea and malabsorption. Other types of persistent inflammation include non-infectious arthritis, gingivitis, and glomerulonephritis. Keratitis and uveitis are two ocular symptoms of CGD. Autoimmune diseases appear to be more common in X-linked female carriers. The most common skin signs are photosensitivity, discoid/malar rash, and the Raynaud phenomenon.
Genes and mutations
CGD pathogenesis is mediated by six genes with two distinct inheritance patterns. These are – CYBB, CYBA, CYBC1, NCF1, NCF2, and NCF4. The most common form of CGD is the X-linked form, caused by mutations in the CYBB gene – found on the X chromosome and codes for NOX2. X-CGD affects almost two-thirds of all CGD patients, the majority of whom are men. Autosomal genes encode p22phox (CYBA), p47phox (NCF1), p67phox (NCF2), and p40phox (NCF4). NCF1 (located on chromosome 7) mutations are detected in approximately 20% of CGD patients. CYBA and NCF2 mutations in around 5% of CGD patients, and NCF4 mutations are uncommon.

Image Credit: Anusorn Nakdee/Shutterstock.com
CYBB mutations range from single nucleotide changes to megabase deletions. Missense, nonsense mutations (direct or by frameshift) produce a stop codon farther downstream, causing protein synthesis to be terminated prematurely. Insertions in CYBB are uncommon. The majority of them are caused by lesser or bigger duplications.
NADPH complex
The active NADPH oxidase complex is a six-protein complex. It has two components in its basic state: a membrane-bound complex embedded in the walls of secondary granules and separate cytosolic components.
The NADH oxidase enzyme is a multicomponent enzyme that consists of a membrane-bound, heterodimeric b-type cytochrome that includes the subunits gp91phox (also known as Nox2) and p22phox. The components of the cytosol are p47phox, p67phox, p40phox, and RAC. The recently discovered EROS (encoded by CYBC1) is necessary for cytochrome b558 assembly and transport. All of these elements are essential for the normal production of superoxide.
Diagnosis and treatment
CGD is diagnosed using direct detection of superoxide production, chemiluminescence, ferricytochrome c reduction, NBT reduction, and the flow cytometry-based test dihydrorhodamine oxidation are examples of these (DHR). Gene mutation study, which is also required for genetic counseling, should be used to confirm abnormal DHR neutrophil assay results. Carrier family members can be identified via genetic and prenatal testing.
Patients with CGD who have acute infections are treated with antibiotics or antifungal medications. Treatment often necessitates surgical draining (and excision) of diseased lymph nodes and abscesses affecting the liver, skin, rectum, kidney, and brain, particularly for visceral abscesses. Most patients require prophylactic antibacterial treatment with trimethoprim/sulfamethoxazole and prophylactic antifungal treatment with itraconazole during infection-free periods (or voriconazole). Corticosteroids can treat granulomatous disease and associated inflammatory consequences. TNF- antagonist infliximab has been demonstrated to be effective in the treatment of CGD-associated colitis.
At present, allogeneic hematopoietic stem cell transplantation is the only curative treatment for CGD patients (HSCT). Gene therapy can be a good option to HSCT for patients who do not have an HLA-compatible donor.
References
-
Yu, H. H., Yang, Y. H., & Chiang, B. L. (2021). Chronic Granulomatous Disease: a Comprehensive Review. Clinical reviews in allergy & immunology, 61(2), 101–113. https://doi.org/10.1007/s12016-020-08800-x
-
Leiding, Jennifer W. (2020). Stiehm's Immune Deficiencies || Chronic granulomatous disease. 829–847. doi:10.1016/B978-0-12-816768-7.00037-5
-
Anjani, G., Vignesh, P., Joshi, V., Shandilya, J. K., Bhattarai, D., Sharma, J., & Rawat, A. (2019). Recent advances in chronic granulomatous disease. Genes & diseases, 7(1), 84–92. https://doi.org/10.1016/j.gendis.2019.07.010
-
Arnold, D. E., & Heimall, J. R. (2017). A Review of Chronic Granulomatous Disease. Advances in therapy, 34(12), 2543–2557. https://doi.org/10.1007/s12325-017-0636-2
-
Roos D. (2016). Chronic granulomatous disease. British medical bulletin, 118(1), 50–63. https://doi.org/10.1093/bmb/ldw009
-
Chiriaco, M., Salfa, I., Di Matteo, G., Rossi, P., & Finocchi, A. (2016). Chronic granulomatous disease: Clinical, molecular, and therapeutic aspects. Pediatric allergy and immunology : official publication of the European Society of Pediatric Allergy and Immunology, 27(3), 242–253. https://doi.org/10.1111/pai.12527
Further Reading
- All Immunology Content
- What is Immunology?
- What does it mean to be Immunocompromised?
- Classical Immunology
- The Immunological Functions of Red Blood Cells
More…
Last Updated: May 2, 2023
Source: Read Full Article