A new study conducted by researchers from Regenstrief Institute and the universities of South Carolina and Indiana has found that the most commonly prescribed blood pressure medications, taken for at least six months prior to an intensive care unit (ICU) admission, did not protect against developing delirium in the ICU, regardless of patient age, gender, race, co-morbidities or insurance status.
Delirium, an acute brain failure, affects approximately seven million hospitalized patients in the U.S. annually and is associated with longer hospital and ICU length of stay, higher likelihood of mechanical ventilation, long-term cognitive impairment, new nursing home placement and greater likelihood of death. As delirium severity and duration increase, post-discharge cognitive and functional outcomes worsen.
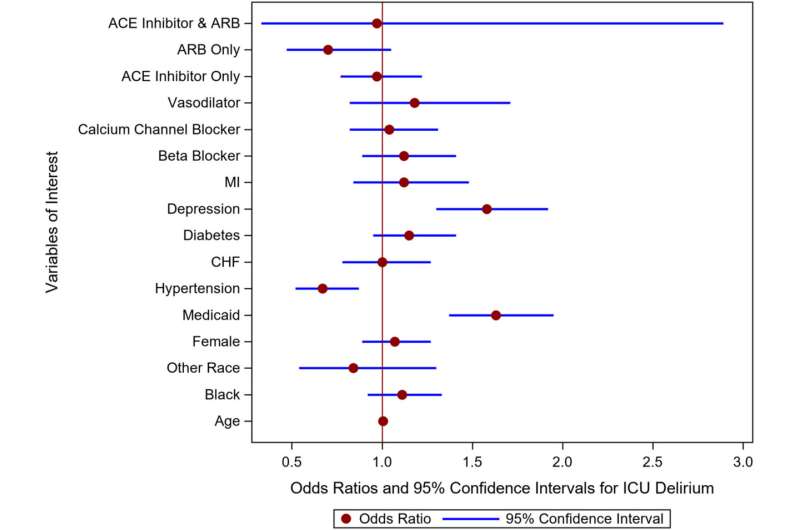
“We have been looking at potential ways to decrease delirium severity and duration. In this study we looked at ACE inhibitors and angiotensin receptor blockers because these drugs stabilize blood pressure and are thought to have neuroprotective qualities. We wanted to learn whether chronic exposure to these drugs may be important in preventing delirium,” said study senior author Babar Khan, M.D., M.S., a Regenstrief Institute and Indiana University School of Medicine researcher-clinician.
“Unfortunately, we did not find lower prevalence of delirium among patients prescribed these medications prior to ICU admission, compared to patients who had not taken them.”
Chronic high blood pressure, which can be successfully lowered by ACE inhibitors and angiotensin receptor blockers, is one of the risk factors for ICU-acquired delirium.
The observational study of the electronic health records of 4,791 racially diverse patients showed that taking these blood pressure medications for at least six months prior to admission to an ICU did not provide enough protective benefit or generate enough brain resilience to prevent delirium.
In other work that looked at a pharmacological approach to delirium, Dr. Khan was a co-author of a study published in the New England Journal of Medicine in 2018 which found that commonly prescribed antipsychotic drugs did not alter duration of delirium.
In the continued quest to identify therapies to prevent or manage delirium, he and fellow Regenstrief Institute and IU School of Medicine faculty member Sikandar Khan, D.O., M.S., are currently collaborating with the Mayo Clinic on a multi-site study to determine if a specially designed music intervention can reduce the likelihood of mechanically ventilated older adult ICU patients developing delirium and can also improve post-ICU brain health.
“This study of blood pressure medications represents our ongoing efforts to understand the role of vascular risk factors in delirium. Our long-term goal is to understand how different biological processes in aging, such as blood pressure, inflammation etc., interact, eventually leading to delirium and then ultimately dementia,” said Dr. Sikandar Khan.
“Relationship between angiotensin-converting enzyme inhibitors and angiotensin receptor blockers prescribing and delirium in the ICU-A secondary analysis” is published in the Journal of the American Geriatrics Society.
More information:
Malissa A. Mulkey et al, Relationship between angiotensin‐converting enzyme inhibitors and angiotensin receptor blockers prescribing and delirium in the ICU‐A secondary analysis, Journal of the American Geriatrics Society (2023). DOI: 10.1111/jgs.18285
Journal information:
Journal of the American Geriatrics Society
,
New England Journal of Medicine
Source: Read Full Article