In a recent study published in the journal PLOS Pathogens, researchers in the United States evaluated a novel self-amplifying replicon ribonucleic acid (RNA) vaccine against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) using pigtail macaques with coronavirus disease 2019 (COVID-19).
The unprecedented morbidity and mortality caused by the COVID-19 pandemic led to the rapid development of vaccines against SARS-CoV-2. Despite extensive vaccination coverage, the health burden of COVID-19 continues to grow due to the continual emergence of increasingly transmissible and immune-evasive SARS-CoV-2 variants of concern (VOCs) and the waning of humoral immunity gained from COVID-19 vaccines or previous SARS-CoV-2 infections. Therefore, novel therapeutics are required to broaden the therapeutic landscape of COVID-19.
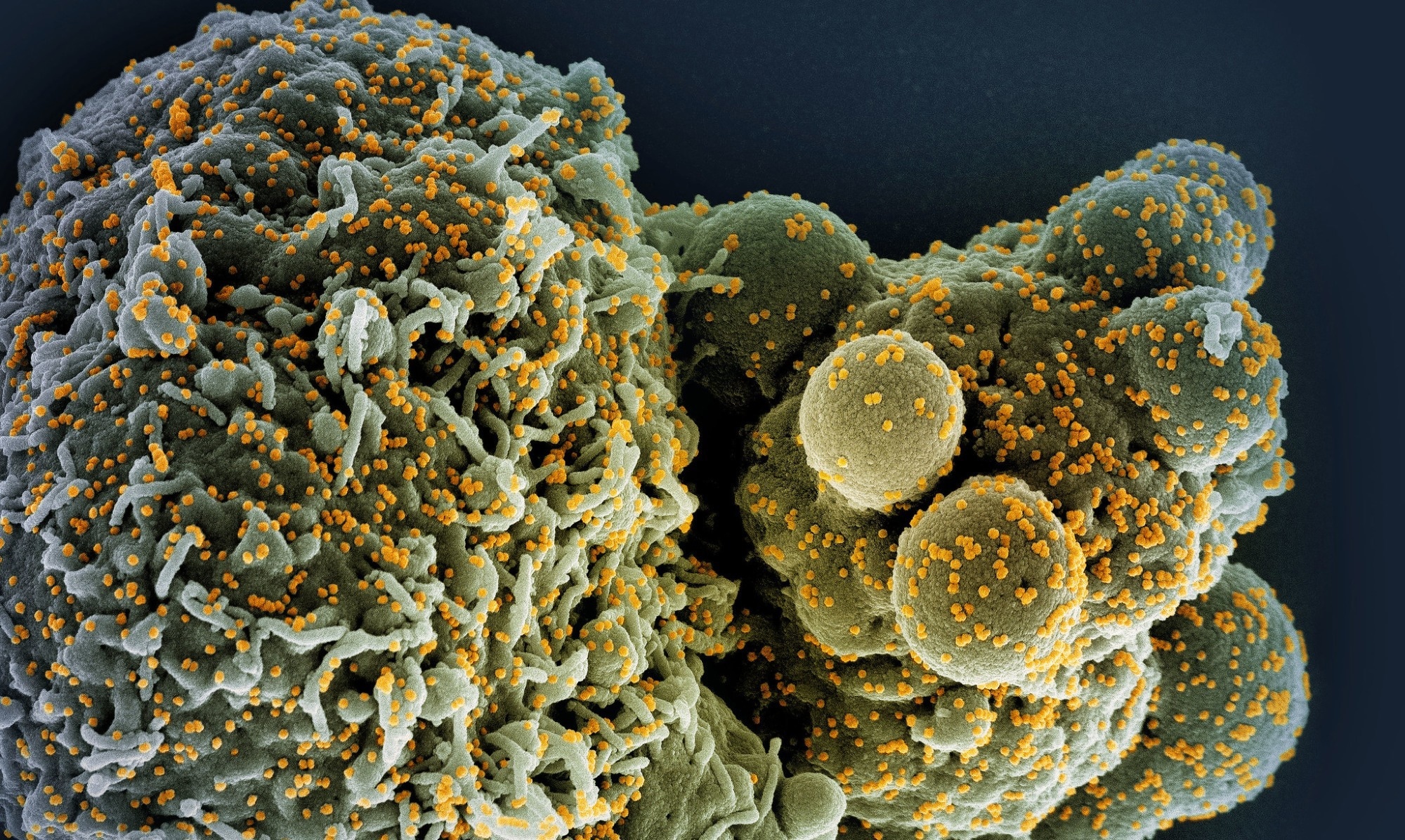 Study: A replicon RNA vaccine can induce durable protective immunity from SARS-CoV-2 in nonhuman primates after neutralizing antibodies have waned. Image Credit: NIAID
Study: A replicon RNA vaccine can induce durable protective immunity from SARS-CoV-2 in nonhuman primates after neutralizing antibodies have waned. Image Credit: NIAID
About the study
In the present study, researchers evaluated the efficacy of a new self-amplifying replicon RNA (repRNA) COVID-19 vaccine among non-human primates.
The team investigated the immune protection conferred by an α-virus-extracted replicon ribonucleic acid (repRNA) vaccine coding for the SARS-CoV-2 spike (S) glycoprotein (repRNA-CoV2S) among vaccinated pigtail macaques when neutralizing antibody (nAb) responses were at their peak and after they had waned. The team evaluated the minimum dosage, the volume of delivery, and the dosing interval that would most probably work among humans. A dose de-escalation strategy was used, wherein individuals’ enrollment was staggered so that data obtained for one study cohort could be utilized to aid in deciding the vaccination regimen for the next group of individuals.
Immunological responses among the 50.0 μg dosage group were compared to those of another group of vaccinated non-human primates boosted with 25.0 μg dosages, administered over an interval of 20.0 weeks. Further, priming and boosting with a 5.0 μg vaccine dose, administered at an interval of six weeks, was investigated. Cross-protective binding antibody (bAb) responses against the S proteins of SARS-CoV-2 VoCs were measured using enzyme-linked immunosorbent assays (ELISA). The nAb titers were measured using the 80.0% plaque-reduction neutralization test (PRNT80).
Serological anti-S interferon-gamma (IFN-γ)-secreting T lymphocyte responses were measured by performing ELISPOT assays using peripheral blood mononuclear cell (PBMC) isolates. Viral load was measured using nasal swab specimens, obtained on days 1.0, 3.0, 5.0, and 7.0; using bronchial alveolar lavage (BAL) samples obtained on days 3.0, 5.0, and 7.0; and pulmonary tissue specimens obtained on day 7.0 post-SARS-CoV-2 challenge. Subgenomic SARS-CoV-2 RNA levels were determined using quantitative reverse transcription-polymerase chain reaction (qRT-PCR).
Results
The self-amplifying repRNA vaccine induced strong bAb and nAb responses against the homologous SARS-CoV-2 strain. In addition, the team observed broad bAbs against the ancestral strain and several VOCs, whereas nAb titers were observed primarily against the ancestral Wuhan-Hu-1 strain. Despite the reduction in nAb titers to negligible levels within seven months of vaccination, sustained bAb titers and swift anamnestic recall responses were observed, which could mediate immune protection against SARS-CoV-2 infection and pulmonary disease following the viral challenge.
The findings indicated that protective immune memory to SARS-CoV-2 vaccination persists, and rapid immunological recall responses could protect against SARS-CoV-2, even in the absence of detectable nAb titers. The team evidenced lowered SARS-CoV-2 multiplication and less severe pathological changes among respiratory organs, reduced shedding of SARS-CoV-2 in nasal cavities, and reduced pro-inflammatory cytokine levels in the pulmonary tissues.
Various vaccine dosages and different vaccination regimens could protect the primates against SARS-CoV-2 infection. In addition, a few macaques were protected even in the absence of neutralizing antibodies at the time of the SARS-CoV-2 infection. Therefore, even when detectable nAb titers were lacking during exposure to SARS-CoV-2, other immunological pathways might regulate immunity levels, including T lymphocytes and binding antibodies.
A 250.0 μg dosage of the vaccine-elicited robust immunological responses following one vaccination only. The dosage was used initially to assess vaccine immunogenicity and safety at the highest dose feasible. A single 25.0 μg booster dose elicited anti-SARS-CoV-2 S immunoglobulin G (IgG) antibodies at six weeks following vaccination that conferred similar humoral immune protection among macaques as two 50.0 μg dosages administered 28.0 days apart. The Ab titers following one vaccine dose continued to rise such that booster dose administration within four weeks of the prime dose might not provide additional immune benefits.
A longer dosing interval between prime and booster vaccinations might induce more robust immunological responses. Further, cross-protective binding antibodies were observed against S proteins of SARS-CoV-2 VOCs such as Alpha VOC, Beta VOC, Delta VOC, Omicron BA.2 VOC, BA.5 VOC, and the BQ.1.1 VOC, but not against Omicron BA.4/5 and Omicron BQ.1.1 VOCs, among the macaques following prime vaccination. Further, IgG titers measured two weeks following the 5.0 μg dose prime and booster vaccinations yielded comparable IgG titers.
The 25.0 μg dose adequately induced maximal T lymphocyte responses, and booster vaccination improves T lymphocyte responses; however, the 5.0 μg dose might be below the cutoff required for significantly inducing T lymphocytes in peripheral blood. The analysis showed that the 5.0 μg dose is sub-optimal for inducing nAb responses, and a longer interval between the prime and booster vaccinations would confer more durable and robust immune protection.
Overall, the study findings showed that among non-human primates, the repRNA vaccine could confer long-term immune protection against SARS-CoV-2, even in the presence of negligible nAb responses.
- O’Connor MA, Hawman DW, Meade-White K, Leventhal S, Song W, Randall S, et al. (2023) A replicon RNA vaccine can induce durable protective immunity from SARS-CoV-2 in non-human primates after neutralizing antibodies have waned. PLoS Pathog 19(4): e1011298. DOI: https://doi.org/10.1371/journal.ppat.1011298, https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1011298
Posted in: Medical Research News | Disease/Infection News | Pharmaceutical News
Tags: Antibodies, Antibody, Blood, Cell, Coronavirus, Coronavirus Disease COVID-19, Cytokine, Efficacy, ELISA, Enzyme, Glycoprotein, Homologous, immunity, Immunoglobulin, Interferon, Interferon-gamma, Lymphocyte, Mortality, Omicron, Pandemic, Polymerase, Polymerase Chain Reaction, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, T Lymphocyte, Therapeutics, Transcription, Vaccine, Virus

Written by
Pooja Toshniwal Paharia
Dr. based clinical-radiological diagnosis and management of oral lesions and conditions and associated maxillofacial disorders.
Source: Read Full Article