A new research paper titled “Novel inflammation-combined prognostic index to predict survival outcomes in patients with gastric cancer” has been published in Oncotarget.
In vivo inflammatory responses are involved in cancer growth, invasion and metastasis, and the involvement of systemic inflammatory responses and the surrounding microenvironment is intricately intertwined. In this recent study, researchers Noriyuki Hirahara, Takeshi Matsubara, Shunsuke Kaji, Hikota Hayashi, Yohei Sasaki, claritin regular strength Koki Kawakami, Ryoji Hyakudomi, Tetsu Yamamoto, and Yoshitsugu Tajima from Shimane University Faculty of Medicine and Matsue Red Cross Hospital in Japan focused on the lymphocyte-to-monocyte ratio (LMR), neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR), and devised an inflammation-combined prognostic index (ICPI) as a prognostic marker of cancer-specific survival (CSS).
The researchers write, “We reviewed the clinicopathological data of 480 patients with gastric cancer undergoing curative laparoscopic gastrectomy between 2009 and 2019. This study examined the significance of LMR, NLR, PLR, and ICPI as cancer-specific prognostic markers.”
In univariate analysis, tumor diameter, histological differentiation, pathological tumor-node-metastasis (pTNM) stage, LMR, NLR, PLR, C-reactive protein (CRP) level, carcinoembryonic antigen (CEA), and postoperative chemotherapy were significantly associated with CSS. In multivariate analysis, pTNM stage and CEA were the independent risk factors for CSS, although LMR, NLR, and PLR were not the independent risk factors for CSS.
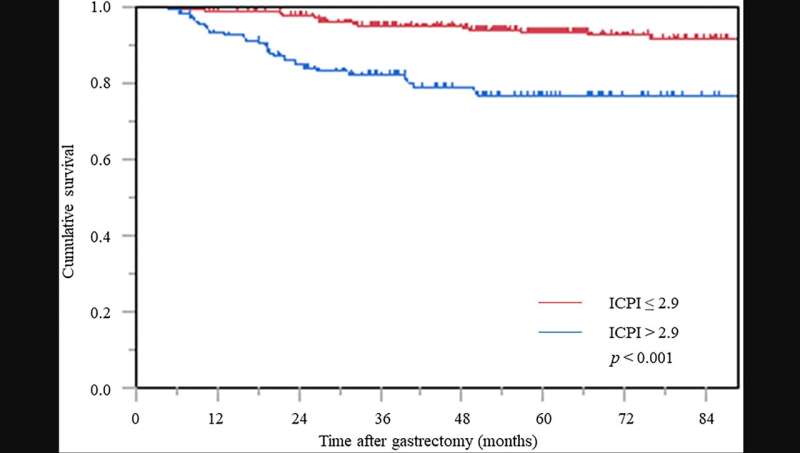
The ICPI formula was constructed using hazard ratios for three inflammation-based biomarkers with worse prognosis identified in the univariate analysis: LMR <4.315, NLR ≥2.344, and PLR ≥212.01, which were each scored as 1, with all remaining values pointed at 0. ICPI was calculated as follows: ICPI = 2.9 × LMR + 2.8 × NLR + 2.8 × PLR. The optimal cutoff value of ICPII was 2.9. On multivariate analysis, pTNM stage, CEA, and ICPI were independent prognostic factors for CSS. In the Kaplan-Meier survival analysis, CSS in the high ICPI group was significantly worse than that in the low ICPI group. ICPI was devised as a novel predictive index for prognosis, and its usefulness was clarified.
“In this study, the ICPI was devised as a novel predictive index of prognosis, and its usefulness was clarified. However, it is still unclear how active preoperative intervention using the ICPI as an indicator will contribute to improved oncological prognosis. In the future, it will be necessary to conduct a multicenter prospective study to examine the prognostic effect of preoperative interventions, including nutrition,” the researchers explain.
More information:
Noriyuki Hirahara et al, Novel inflammation-combined prognostic index to predict survival outcomes in patients with gastric cancer, Oncotarget (2023). DOI: 10.18632/oncotarget.28353
Journal information:
Oncotarget
Source: Read Full Article