In a recent study posted to the bioRxiv* preprint server, researchers evaluated neuro-pathophysiological consequences of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, especially the post-acute sequelae of SARS-CoV-2 (PASC) in Alzheimer’s disease (AD) patients.
About the study
In the present study, researchers collected the Broadman area 9 (cortical BA9) and hippocampal formations (HF), the central nervous system (CNS) regions with the most significance in AD, of four SARS-CoV-2 cases, four AD cases, and four non-SARS-CoV-2 or AD autopsies done at the neuropathology brain bank and research CoRE at Mount Sinai in New York City, United States. The team compared transcriptional and cellular responses in these two brain regions, deeply involved in cognitive and emotional functions, to age- and gender-matched neurological cases.
Each study cohort comprised an equal number of age-matched male and female patients, with an average age of 79.6 years. The team confirmed SARS-CoV-2 infection by diagnostic reverse transcription-polymerase chain reaction (RT-PCR). Within the SARS-CoV-2 and SARS-CoV-2 infected AD groups, all patients were symptomatic, admitted to the hospital, and received oxygen supplementation. Patients with SARS-CoV-2 and SARS-CoV-2 infected AD patients died on average 27 and 32 days from disease onset, respectively. The team also collected and tested blood specimens of these patients [e.g., for C-reactive protein (CRP)], the results of which indicated severe coronavirus disease 2019 (COVID-19).
Likewise, all AD individuals had postmortem ABC scores indicative of AD, where A is a measure of amyloid-beta deposition. Likewise, B and C scores are measures of neurofibrillary degeneration based on the Braak and Brook score and neuritic plaques outlined by the Consortium to Establish a Registry for AD diagnosis (CERAD), respectively.
For each case, the team used one brain hemisphere to make formalin-fixed paraffin-embedded (FFPE) tissues and froze the others to generate fresh-frozen blocks. They used the former for microscopy and the region-matched later for sequencing. All tissue harvesting adhered to the Institutional Review Board (IRB) guidelines.
The researchers collected, homogenized, and processed all brain tissue samples to collect total ribonucleic acid (RNA). Likewise, they cut FFPE brain tissue sections of 6µm on a Leica Microtome for immunohistochemistry (IHC) analyses. IHC analyses fetched evidence of microglial activation via the presence or absence of allograft inflammatory factor 1 (Iba 1), SARS-CoV-2 nucleocapsid (N), and vascular integrity, assessed via hypoxia-inducible factor-1 subunit (HIF-1α). The researchers used hematoxylin-stained nuclei to quantify the total number of microglial cells and those with Vector Red intensity above a rigorous threshold (Iba-1+). They reported microglia frequency as the percentage of total nuclei in the tissue section assessed.
Study findings
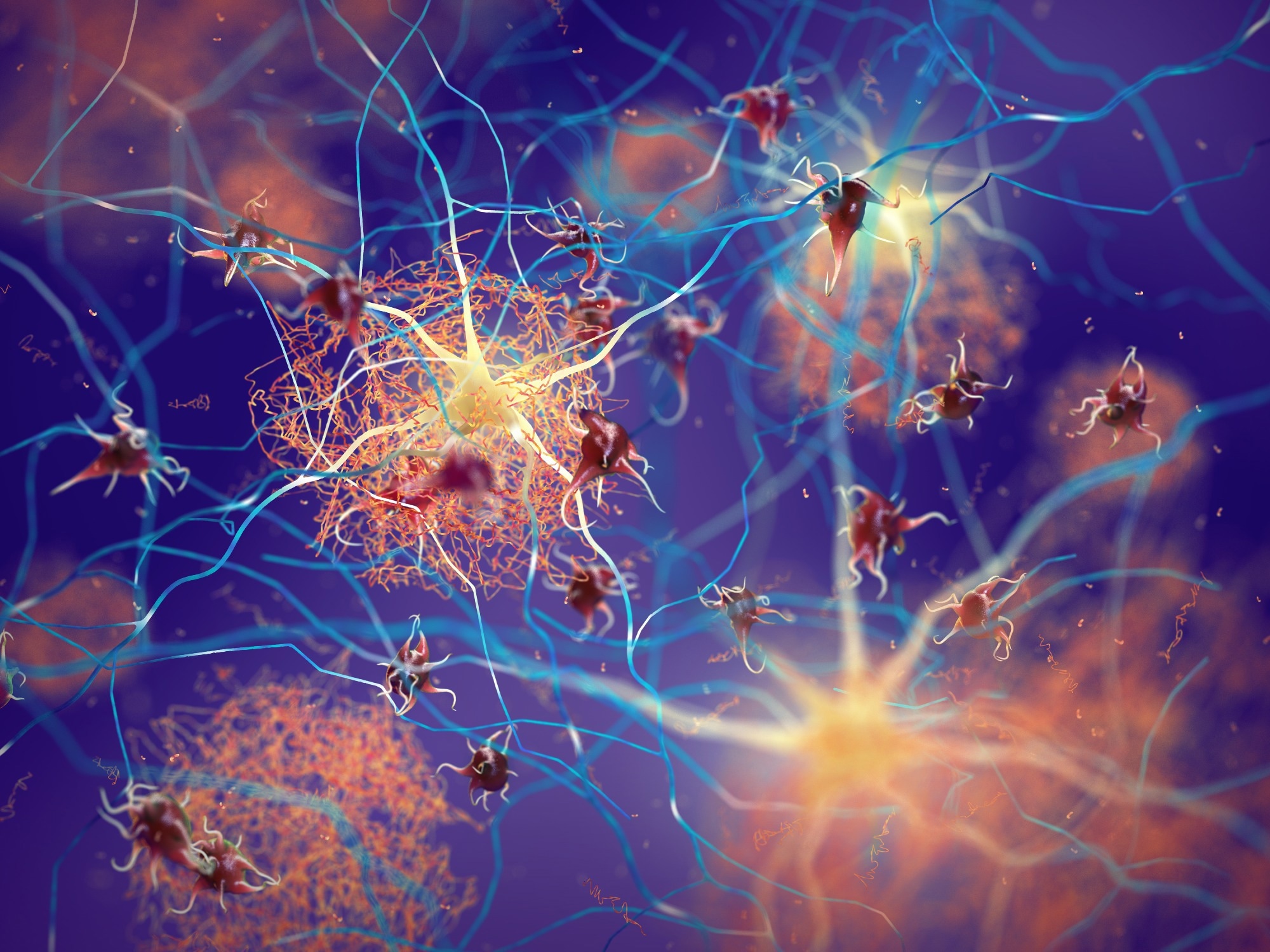
Compared to neurological control brains, microglia in AD, SARS-CoV-2, and SARS-CoV-2 infected AD cases were more numerous, accumulated around blood vessels, and displayed retracted, thickened processes and enlarged somas, suggesting factors at the level of the BBB might be participating in microglial activation. The researchers found microglial nodules in all groups, but they appeared larger and more frequent in SARS-CoV-2 infected than in AD and control groups. Moreover, SARS-CoV-2 appeared restricted to the endothelium and did not co-localize with Iba-1 or glial fibrillary acidic protein (GFAP), suggesting neither microglia nor astrocytes harbored the infectious virions.
Neuroscience eBook

Non-biased quantitation revealed an overall increase in microglia in the HF and cortical BA9 of all three study groups. However, this increase was statistically significant in the HF of AD cases; and both HF and cortical BA9 of SARS-CoV-2 infected AD cases. Likewise, both brain regions showed an increased frequency of nodular lesions with SARS-CoV-2 infection, with and without AD. However, this increase was also statistically significant in SARS-CoV-2-infected AD cases.
Regardless of AD status, SARS-CoV-2-infected individuals had significantly upregulated HIF-1α levels in the same brain regions. Microglia nodule formation is present in other neurodegenerative diseases and viral infections, such as multiple sclerosis (MS) and herpes simplex virus (HSV). Likewise, AD patients with SARS-CoV-2 infection had nodular morphological alterations in the brain due to changes in the distribution of microglial cells, reflected by the increase of Iba 1.
Further, the increased nodular formation in SARS-CoV-2-infected AD cases led to increased toll-like receptor (TLR) signaling and upregulation of inflammasome genes. It led to T cell stimulation and the destruction of neurons, suggesting SARS-CoV-2 further promoted neuroinflammation in AD, which likely advanced the progression and severity of CNS disease in these individuals. Consistent with the findings of Zhou et al., the researchers also found a significant overlap in cerebrospinal fluid (CSF) monocytes and markers in AD and SARS-CoV-2 groups.
Another large retrospective study on patients 65 years or older revealed that patients with SARS-CoV-2 were at an increased risk for a new AD diagnosis within a year of COVID-19 diagnosis, with the most significant risk seen among those 85 years and older. SARS-CoV-2 promotes preexisting inflammation in the brain, seen due to ‘normal’ aging, and advances AD progression. Furthermore, the researchers noted changes in the transcriptional regulation of soluble N-ethylmaleimide-sensitive factor activating protein receptor (SNARE) and nerve growth factor (NGF) pathways, suggesting impaired neuronal health and function, presumably negatively impacting cognitive functions. They also observed potential damage to the vasculature via increased regulation of HIF-1α, integrin signaling, and IL-8 signaling.
The SARS-CoV-2 N protein remained limited to the endothelium, suggesting that the hematological spread of SARS-CoV-2 to the CNS induced widespread inflammation in the brain despite not extending to the neurons in the cortical BA9 and HF. Another intriguing observation of the current study was that SARS-CoV-2 impacted cognitive dysfunction even when it remained undetected in the neurons. SARS-CoV-2 used triggering receptor expressed on myeloid cells 1 (TREM1) activation of the NLR family pyrin domain containing 3 (NLRP3) inflammasome. Pro-caspase 1 cleavage and subsequent activation of IL-1β, IL-18, and gasmerdin D pore formation in cells ultimately led to pyroptosis. Studies have reported NLRP3 activation in AD and COVID-19, and the formation of microglial nodules observed in these cases supported the same.
Conclusions
The current study demonstrated that SARS-CoV-2 infection promoted similar pathophysiological features in cortical BA9 and HF regions as in AD cases. It also possibly exacerbated preexisting AD pathophysiology. However, it recapitulated SARS-CoV-2-triggered AD-type transcriptional and cellular neuroinflammatory patterns in a short time frame. It would be interesting to decipher how SARS-CoV-2 impacts long-term cognition. The observed increase in nodular formation in SARS-CoV-2- infected AD cases also highlight the need to determine the potential synergistic effects of AD and SARS-CoV-2 at the functional level.
To conclude, during COVID-19 and AD, similar neuro- and immune-inflammatory pathways and processes, especially those involved with cognition, were affected, which explains the neuro-pathophysiological consequences observed during PASC, such as brain fog and memory loss.
*Important notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Elizabeth Griggs, Kyle Trageser, Sean Naughton, Eun-Jeong Yang, Brian Mathew, Grace Van Hyfte, Linh Hellmers, Nathalie Jette, Molly Estill, Li Shen, Tracy Fischer, Giulio Pasinetti. (2022). Molecular and cellular similarities in the brain of SARS-CoV-2 and Alzheimer's disease individuals. bioRxiv. doi: https://doi.org/10.1101/2022.11.23.517706 https://www.biorxiv.org/content/10.1101/2022.11.23.517706v1
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: Aging, Alzheimer's Disease, Blood, Blood Vessels, Brain, Brain Fog, Cell, Central Nervous System, Coronavirus, Coronavirus Disease COVID-19, covid-19, C-Reactive Protein, Diagnostic, Frequency, Genes, Growth Factor, Herpes, Herpes Simplex, Herpes Simplex Virus, Hospital, Hypoxia, IHC, Immunohistochemistry, Inflammasome, Inflammation, Microglia, Microscopy, Microtome, Multiple Sclerosis, Nerve, Nervous System, Neurodegenerative Diseases, Neurons, Oxygen, Pathophysiology, Polymerase, Polymerase Chain Reaction, Protein, Receptor, Research, Respiratory, Ribonucleic Acid, RNA, SARS, SARS-CoV-2, Sclerosis, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Syndrome, Transcription, Vascular, Vasculature, Virus

Written by
Neha Mathur
Neha is a digital marketing professional based in Gurugram, India. She has a Master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. She has experience in pre-clinical research as part of her research project in The Department of Toxicology at the prestigious Central Drug Research Institute (CDRI), Lucknow, India. She also holds a certification in C++ programming.
Source: Read Full Article