The ongoing coronavirus disease 2019 (COVID-19) pandemic has led to over 6.4 million deaths, with fresh cases continuing to emerge. With the widespread vaccination drives, the spread of the virus was expected to decrease. The occurrence of breakthrough infections and reinfections proved this hope wrong.
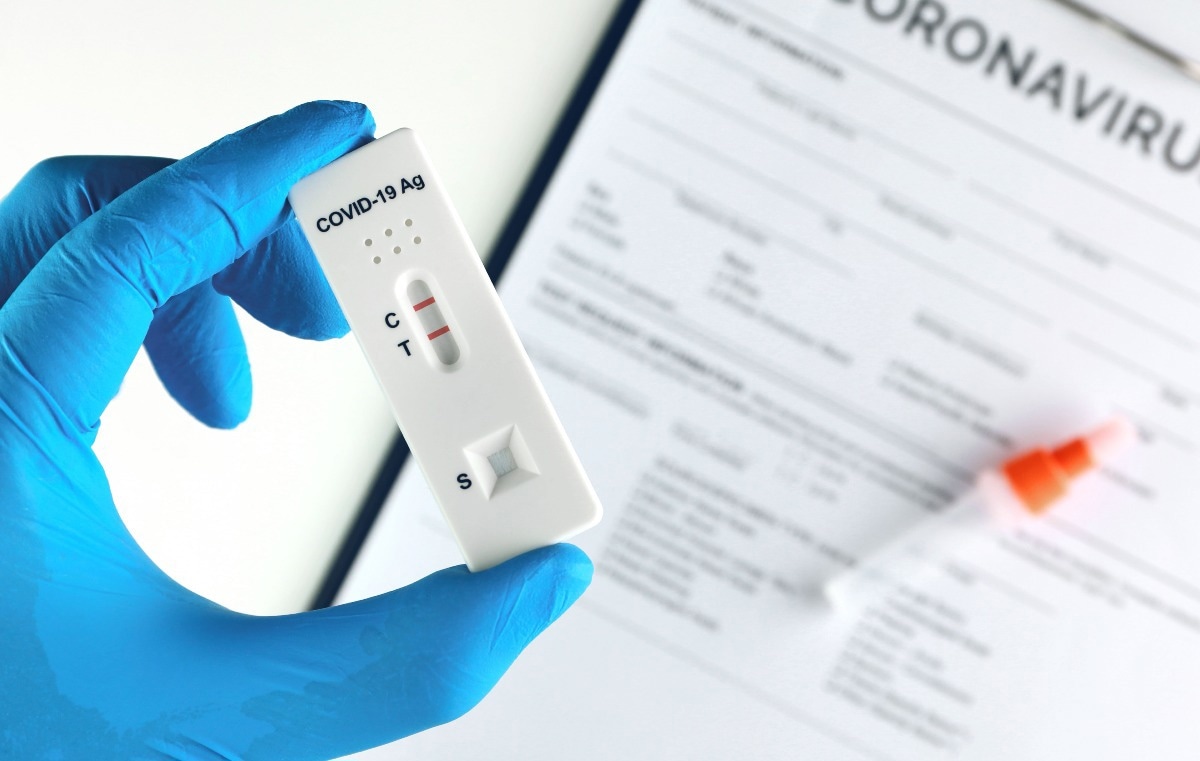
A new study maps the escape mutations found in various strains of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that could cause them to escape neutralization by antibodies or detection by rapid antigen tests that rely on antibody binding for a positive result.
Introduction
Diagnostic tests for COVID-19 were launched as early as April 2020, using in vitro reporting using the viral sequence of the ancestral variant of the virus, the Wuhan variant. With the emergence of new variants, questions have arisen about the performance of these tests, as they exploit the ability of antibodies to recognize and bind to the viral antigens. This recognition is subverted in the presence of escape mutations.
The current study, published in the journal Cell, presents a new method to assess the impact of such N target mutations on antigen recognition by diagnostic antibodies used in rapid antigen tests.
Rapid antigen tests help detect the presence of SARS-CoV-2 rapidly and easily. In most cases, they use the viral nucleocapsid (N) antigen, which is present in abundance in viral particles as well as in infected individuals. The N protein is key to the viral life cycle, including viral replication and packaging. It has an RNA binding domain (N-RBD) and a dimerization domain (N-DD), around which there are three disordered regions.
Antibodies bind to epitopes, specific antigen regions that have a complementary structure to the binding domain of the antibody. Epitope mapping is a field that uses multiple techniques, such as structure determination, mass spectrometry, or site-directed mutagenesis, to help identify the escape mutation sites on the antigen. However, none of the methods used at present can directly measure the effect of a given mutation on antibody binding.
Many researchers are turning to deep mutational scanning (DMS), a method that examines most or all the mutations in a protein via a library of mutants or unique sequences. These sequences can be simultaneously screened using in vitro selection techniques to enrich the relevant mutations.
When used alongside cell surface display methods, DMS has helped study SARS-CoV-2 spike protein interactions with the host angiotensin-converting enzyme 2 (ACE2) receptor and the key mutations that disrupt spike-antibody binding at the spike RBD.
In the current study, mammalian cells are used for the surface display of the N protein to achieve the direct quantitative antibody binding assay. Combing this with DMS using a library of all possible amino acid substitutions along the full length of the N protein, the researchers were able to perform a complete assay of the effects of all possible mutations on antigen binding to 17 diagnostic antibodies currently used to test for this virus.
The result is a full picture of the escape mutations possible for each antibody, scored for escape potential at each region. The scores show how abundant the given mutation is in the group of cells expressing escape mutations. Thus, it shows how much effect each mutation has on antibody binding.
The scores thus help identify both the epitopes and the susceptibility of the diagnostic antibody to mutations in or near the epitope. The data helps understand how each mutation at these sites affects antibody recognition. In this way, the antibody binding strength over the whole of the N mutational sequence library was measured, accounting for every possible point mutation.
What did the study show?
As expected, most mutations do not reduce antibody binding, this effect being confined to a small set of mutations at well-defined sites. This includes epitopes bound by antibodies like R040, C706, and 3C3. With the first, any mutation at three distinct positions causes reduced binding, but only changes in charged or polar amino acids at another position produce this effect.
The latter two are examples of antibodies binding to 3D epitopes where only a few mutations are significantly associated with markedly reduced antibody binding. With 3C3, an E323 substitution almost always has a large impact, but not at V324, where only mutations in charged or aromatic amino acids cause reduced binding.
Overall, this shows that a given epitope is sensitive to some substitutions but not others and highlights the detailed information available with this platform.
Any mutation at three sites in the epitope of R040, and four sites in the C706 epitope, abolished binding, but outside these epitopes, mutations were insignificant. Interestingly, with 3C3, two mutations abolished binding and another reduced binding affinity by 2 orders of magnitude. A fourth had a mild effect only, but the other two antibodies picked up this mutant at normal binding levels.
This indicates that the partial misfolding of the protein caused by the latter mutation was inadequate to reduce the affinity of binding with these antibodies. Long-range effects on binding were also seen with some N-RBD mutations, indicating that binding may reduce without a noticeable change in affinity.
The study yielded a wealth of information about where antibodies bind to the N protein. It demonstrates how different antibodies escape via their distinctive sets of escape mutations, helping unravel the underlying mechanism of escape and allowing the antibodies to be distinguished even when they bind to overlapping epitopes.
Rapid antigen tests operate based on two antibodies, one in a solid and the other in a mobile phase, with both being required to bind to the antigen for signal generation. Interestingly, the data from this study indicates that these diagnostic sets of antibodies bind to different epitopes, so that both are unlikely to have the same high escape score in a given N protein region. That means that all the antibodies used in these tests can bind simultaneously, validating the reliability of these tests.
Together, these data show that DMS may be used to guide the selection of suitable antibody pairs in the design of new antigen tests.”
Implications
The findings show the value of rapid antigen tests in picking up mutations in both current and older SARS-CoV-2 variants. The N protein mutations known at present are unlikely to cause test failure.
Secondly, by presenting the binding assay results for all possible point mutations, including those that could arise in the future, they are important for further tracking of the evolution of this virus and the development of the pandemic. This is of immense value for clinical and public health management.
Again, this method combining DMS with mammalian cell surface display is superior to the current gold standard, structural epitope mapping, because it directly evaluates antibody recognition of the full-length antigen while using the mutational library to measure binding with any possible mutation.
Even though it does not directly identify the epitope, it provides an antibody-specific escape mutation fingerprint. This can be used more widely to examine how antigenic mutations affect antibody binding. It can be adapted to study protein-protein interactions in general, provided a system can be devised to express the proteins on either side.
Moreover, it can help understand other processes like affinity maturation in the germinal center of B cells, including the increase in antibody affinity as specificity increases and resistance to antigen mutations.
- Frank, F. et al. (2022). Deep mutational scanning identifies SARS-CoV-2 Nucleocapsid escape mutations of currently available rapid antigen tests. Cell. doi: https://doi.org/10.1016/j.cell.2022.08.010. https://www.sciencedirect.com/science/article/pii/S0092867422010443
Posted in: Medical Science News | Medical Research News | Disease/Infection News
Tags: ACE2, Amino Acid, Angiotensin, Antibodies, Antibody, Antigen, Assay, binding affinity, Cell, Coronavirus, Coronavirus Disease COVID-19, covid-19, Diagnostic, Enzyme, Evolution, in vitro, Mammalian Cells, Mass Spectrometry, Mutation, Pandemic, Protein, Public Health, Receptor, Respiratory, RNA, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spectrometry, Spike Protein, Syndrome, Virus

Written by
Dr. Liji Thomas
Dr. Liji Thomas is an OB-GYN, who graduated from the Government Medical College, University of Calicut, Kerala, in 2001. Liji practiced as a full-time consultant in obstetrics/gynecology in a private hospital for a few years following her graduation. She has counseled hundreds of patients facing issues from pregnancy-related problems and infertility, and has been in charge of over 2,000 deliveries, striving always to achieve a normal delivery rather than operative.
Source: Read Full Article