A new research study reveals that Valley Fever, a fungal disease most commonly found in Arizona and California, may be more common in Utah than previously thought.
The study showed that cases of Valley Fever have been slowly increasing, and the disease now affects people in a larger geographical area than previously recognized. This study is the largest, most comprehensive assessment of Valley Fever cases in Utah in more than 50 years.
In a collaborative project, researchers from University of Utah Health, Intermountain Healthcare, and the Utah Department of Health (UDOH) described the clinical characteristics, acid reflux disease symptoms children geographic distribution, and rates of Valley Fever throughout Utah. A 1957 study found Valley Fever in three counties in southwestern Utah: Iron, Kane, and Washington. Over the years, however, the disease hasn’t been closely tracked.
“With climate change, temperatures are increasing,” says Adrienne Carey, M.D., infectious disease specialist at University of Utah Health. “With increased temperatures and drier conditions, the map will change, and it should probably be expected to spread northward. Aside from a highly publicized outbreak in 2001 at Dinosaur National Monument, there really is a lack of data about how common Valley Fever is within the state of Utah.”
Carey led the study in collaboration with Brandon Webb, M.D., infectious disease specialist at Intermountain Healthcare. “This study is important for several reasons,” Webb says. “It highlights that Utah is indeed an area where Coccidioides is endemic and sheds new light on the many ways that Valley Fever can affect patients. It also identifies areas in the state where epidemiologists and doctors should pay close attention for new cases as climate change, population growth, and new development continue to impact the environment where these fungal spores may be hiding.”
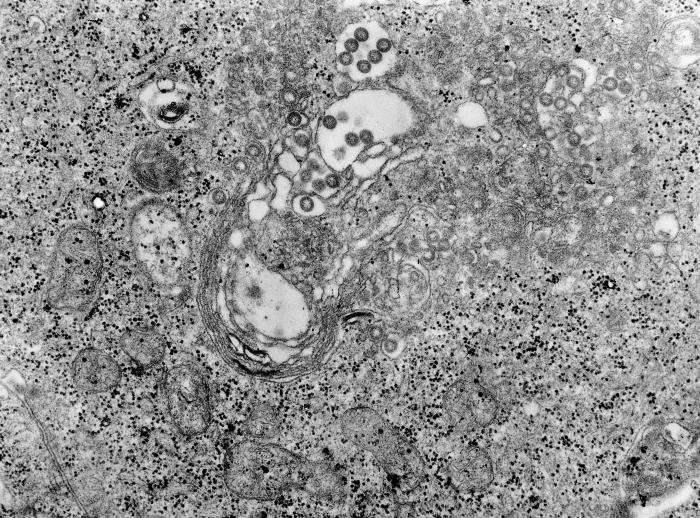
Valley Fever is caused by Coccidioides, a fungus that can infect the lungs. The fungus lives in the soil but becomes airborne when dust is disturbed, such as by construction or high winds. If people inhale that dust, they can become infected, but the disease isn’t contagious from person to person.
The team identified 364 cases of Valley Fever that occurred between 2009-2015 and met the research criteria for “proven” or “probable” Coccidioides infection. They correlated those cases with various environmental factors, including average temperatures, population density, and construction activity, as well as demographic factors like age, race, occupation, and medical issues that could increase vulnerability to infection. The study was published in the peer-reviewed journal Emerging Infectious Diseases, published by the Centers for Disease Control and Prevention (CDC).
The researchers found a higher incidence of the disease since the last report, and even during the seven-year study period, the rate climbed slightly. As before, most cases occurred in the southwestern part of the state, including Washington, Iron, and Kane Counties, plus Garfield and Beaver. This area includes Zion National Park, which attracts more than four million visitors a year, and other recreational areas.
“Interestingly, one of the fastest-growing cities in the United States, St. George, is in southwestern Utah,” Carey points out. “With the rapid growth of construction that’s occurring, there’s increased risk for people to come in contact with the fungus.”
The researchers’ model also predicted a second potential hotspot, in the northeastern part of the state. While cases there are low for now, population growth, increased construction activity, and rising temperatures could create a favorable environment for the fungus to infect more people. Certain groups have an increased risk of contracting the disease, they found, including Black or Filipino people, those with compromised immune systems, and older people.
Statewide, Utah saw two cases per 100,000 people annually, and Washington County had the highest rate, at 17 per 100,000. Most people who encounter Coccidioides don’t get sick, and those who do usually recover without treatment. Symptoms include fever, chills, shortness of breath, and coughing, making Valley Fever difficult to distinguish from more common diseases.
“A delay in diagnosis is common with Valley Fever,” Carey says. “It can cause identical symptoms to bacterial pneumonia. Unless you have a suspicion to test for Valley Fever, you can get tricked and treat somebody with antibiotics.” Antibiotics, which specifically target bacteria, do nothing against a fungal infection.
Valley Fever can also cause nodules that resemble cancer on a chest X-ray, triggering a biopsy. Radiologists and oncologists should be aware of the possibility of Valley Fever, however, so they can consider testing for it.
People who are potentially vulnerable might consider wearing masks to protect themselves from inhaling the fungus spores, particularly in dusty or windy conditions or while participating in outdoor recreation.
These days, any sign of flu-like symptoms prompts fears of COVID-19. But if you have been exposed to a lot of dust, that cough might just be Valley Fever. “If folks are experiencing symptoms like that, they should get tested for COVID,” Carey says. “But also consider Valley Fever if you live in an area where cases are high.”
Source: Read Full Article