Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
As COVID-19 cases surge around the world, life has become complicated for the countless parents sending their young, unvaccinated children back to school. Some public health experts are bracing for more outbreaks of the highly contagious Delta variant, even as a number of US states have tried to bar schools from requiring measures such as mask-wearing, with some noting that children are at low risk from the virus.
Scientists are also wondering what the surge means for children. And they are wondering, too, what those kids stand to teach them. Why is COVID-19 so much worse in adults? Could children’s biology hold clues for defeating the virus? The questions are difficult to study, and evidence is muddled by the emergence of new variants. But researchers are beginning to assemble the pieces of biological data and societal patterns that could explain why children are largely spared.
Here’s a look at lessons learned so far.
Has COVID Been a Problem for Children?
Overall, kids have been lucky with the pandemic: Although it’s not yet clear whether they are less likely than adults to contract or transmit COVID-19, they are far less likely to get sick. According to the Centers for Disease Control and Prevention, as of August 25 only about 400 children under 18 have died of the disease in the US. And, of the two dozen states reporting in addition to New York City, just 0.1% to 1.9% of children who tested positive for the virus have been hospitalized. A recent UK study that crowdsourced health information from the public through an app found that only 1.8% of children with COVID-19 still had symptoms 8 weeks after infection.
Still, children have accounted for nearly 15% of all cases in the US since the start of the pandemic — and represent a lot more than that right now: about 22.4% of cases for the week ending August 26. There is no evidence yet that the Delta variant is more dangerous to kids than previous versions of the virus, but vaccines are not yet available for children under 12, many places have loosened public health restrictions, and Delta is so contagious that it is spreading rapidly. An average of 350 kids under age 18 per day were hospitalized the week of August 24 to August 30, and children’s hospitals in some states have run out of beds.
Why Don’t Children Get as Sick as Adults?
Part of the explanation for kids’ resilience may lie in their overall health. Children are less likely to have conditions like obesity and diabetes, which increase the likelihood of severe COVID-19.
But biology is at play too. Kids’ nasal passages appear to contain less of the ACE2 receptor that the coronavirus uses to get into cells, and airway cells show differences that may prime them to detect the virus early. And children’s immune systems are less developed, which may actually provide an advantage. Severe COVID-19 cases and deaths are thought to be often caused not by the coronavirus itself but by an inflammatory overreaction in which the immune system attacks the lungs. This “cytokine storm” is less common in children than in adults.
The story may be more complex, though, because children’s immune systems are fundamentally unlike those of adults, in ways that are still under study. Scientists know, for example, that the novel coronavirus isn’t the only pathogen to prove much less harmful to children. Adults tend to get much sicker from diseases like hepatitis and mumps; kids with hepatitis often show no symptoms at all.
Yet for some other viruses, the opposite is true. The flu is more dangerous for young children than for healthy adults under age 65, as is respiratory syncytial virus (RSV). In those cases, the more someone is exposed to the viruses over the course of their lives, the stronger their immune response becomes. That makes it easier to fight off an infection in the future.
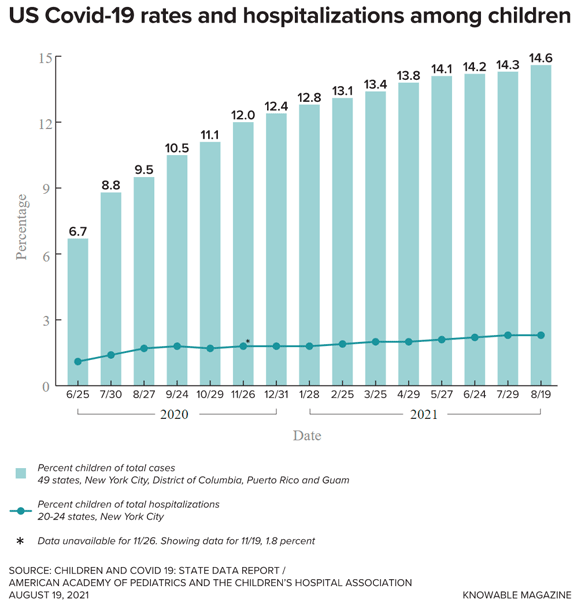
Children represent a small fraction of identified US COVID-19 cases, as shown in this graph. But that all-time percentage has steadily inched up due to an increased proportion of child COVID cases more recently: In the week ending August 26, 2021, children represented about 22.4% of US COVID cases. The chart also shows that hospitalization rates for children who test positive for the virus are very low.
A major immunological difference may help to explain these facts. Compared with adults, kids have more “naive” versions of T cells, which are tailored to recognize specific pathogens. By the time a person reaches their 30s, many of these naive cells will have encountered pathogens and turned into “memory” T cells that can respond much more quickly should they encounter that same, or similar, pathogen again.
At the same time, the body’s production of naive cells slows down. So when a completely new pathogen like SARS-CoV-2 — the cause of COVID-19 — comes along, adults don’t have as many naive cells to recognize and respond to the new threat. “For kids, that’s all they have,” says immunologist Donna Farber of Columbia University. “In some ways, they’re a lot more adapted to see a new pathogen.”
Still, Farber thinks there’s a more important reason why kids are relatively resistant to SARS-CoV-2. Probably, she says, the coronavirus is largely mopped up before those specialized T cells are on the scene. That mopping is done by another branch of the immune system that also differs between young and old: the innate immune system, which includes cells like macrophages and neutrophils that engulf foreign invaders and debris. This system of rapidly responding cells tends to become less efficient as people age.
A 2020 study offers support to that idea. Tracking a group of adults and children with COVID-19, it found that the blood of kids and youth under 24 contained higher levels of cytokine proteins called IL-17a and IFN-γ, which instruct the innate immune system to attack. This group also recovered much more quickly than the adults.
And a 2021 study from Farber’s lab found that children with COVID-19 produce fewer types of antibodies against the virus, and smaller amounts of them than adults do. That’s probably because they don’t need to, she says: The innate immune system has already taken care of the infection.
Do Children Really Spread COVID-19 Less Than Adults?
Transmission by children has been extremely difficult to study, not least because many children never show symptoms of the virus at all. In theory, children’s smaller, weaker diaphragms would mean that they don’t puff out virus as far when they breathe or talk, says Danny Benjamin, an epidemiologist at Duke University in Durham, North Carolina. But that’s not how kids behave in real life. “If you cram 30 of them into a small, enclosed room and let them scream at each other for 8 hours a day — otherwise known as elementary school — they are perfectly capable of transmitting the virus,” he says.
Still, if children’s immune systems do fight off the infection quickly, that means they have less virus to spread. One study of more than 2,500 people in Iceland, where the government tries to track every COVID-19 exposure and infection, seems to bear this out. Researchers found that people over 16 years old were nearly 60% more infectious than children.
And though children do still spread the virus, it’s hard to know how important schools are in that transmission chain. “It’s a really difficult question,” says Shamez Ladhani, a pediatric infectious diseases consultant at St. George’s Hospital in London. It’s often hard to tell whether schools are sources of outbreaks or simply reflecting transmission rates in the wider community.
Furthermore, Ladhani says, because most people have been isolated over the past 18 months — a highly unusual situation — the data that do exist specifically from schools don’t reflect the role that children and schools would play in a pandemic if people were moving more freely. After all, many schools still have distancing requirements and children may not be interacting with one another as much in other places because their families are avoiding social contact.
So far, many studies have reported that schools aren’t a major source of transmission. For instance, from March 2021 to June 2021, Benjamin’s team followed more than 1 million elementary school students and staff at North Carolina schools with mask requirements. During this period, more than 7,000 kids and staff with COVID-19 went to school while infectious and exposed more than 40,000 people, who had to quarantine as a result. Yet when the researchers did contact tracing and testing, they found only 363 cases of COVID-19 transmitted at schools during this period. If mask policies are enforced, Benjamin concludes, schools are among the safest public buildings to be in. Several other states and countries whose schools remained open during the pandemic show similar trends.
But the picture may be changing with the highly transmissible Delta variant, which reaches levels in samples that are 1000 times higher than those of the original strain, likely due to much faster replication in the body. “Whatever advantage kids had is now overwhelmed by larger infecting doses,” says Catherine Bennett, an epidemiologist at Deakin University in Australia. Furthermore, Delta is hitting at a time when many places are relaxing restrictions on masks and social distancing. “Everything is changing, and the virus is changing,” she says.
Australia, for example, managed to largely avoid serious COVID-19 outbreaks until recently. Now, outbreaks of the Delta variant in Brisbane and other parts of Queensland appear to be driven by school transmission, for example at sports meets, Bennett says. If Delta is replicating quickly in the body, it could shorten the time between when a person is infected and when it begins to spread, making quarantining difficult, she adds. “By the time you discover a problem in a school, it’s already impacted other schools.”
Why Can’t Kids Under 12 Be Vaccinated Yet?
Regulatory agencies like the US Food and Drug Administration typically move more cautiously when approving treatments for children. Ethical considerations and logistics are more difficult when working with kids. Furthermore, kids are not just mini-adults: Their physiology, hormones and brains differ. Their livers may not metabolize drugs the same way that adult livers do, and treatments that are safe for adults could have unexpected effects on their development. Differences are marked for the immune system and, by extension, researchers expect the effect of vaccines may differ as well, particularly in terms of how long they may offer protection. Still, it’s generally expected that they will be safe and effective in kids.
Adding to the difficulty, the experiences from other, established vaccines are of scant help because many vaccines are specifically given in childhood, not adulthood, making comparisons hard. And in the case of vaccines that are given to all age groups, such as the flu vaccine, adults have already had a chance to mount an immune response because of prior exposures. That isn’t the case for COVID-19.
“There’s a lot to learn about how children and adults respond differently,” Farber says. “It’s a natural experiment, with the entire world all responding to a new pathogen.” It is heartening though, she says, that children ages 12 to 15 appear to have a slightly stronger immune response to the mRNA vaccines than adults do.
To gather more information, the FDA recently asked Pfizer and Moderna to expand the number of 5- to 11-year-olds in their trials to ensure that they will detect any rare side effects. So far, those appear to be minimal in 12- to 18-year-olds — the youngest people who can currently receive the vaccine in the United States.
Regulators are particularly concerned about myocarditis, a heart inflammation condition that has been linked to mRNA vaccines. Data from more than 5 million vaccinated people in Israel showed a small risk of myocarditis — 148 cases — among young men who received Pfizer’s mRNA vaccine. The risk appeared highest in 16- to 19-year-olds. That is largely why the UK has not yet fully approved vaccines for children under 16, Ladhani says. It’s a difficult thing to study, he adds, as myocarditis may not appear immediately or may be so mild as to escape notice.
If the trial goes well, Pfizer and Moderna plan to submit emergency use applications to the FDA that will allow 5- to 11-year-olds to be vaccinated, and the FDA predicts that the vaccines will be available by midwinter.
This article is part of Reset: The Science of Crisis & Recovery, an ongoing Knowable Magazine series exploring how the world is navigating the coronavirus pandemic, its consequences and the way forward. Reset is supported by a grant from the Alfred P. Sloan Foundation.
Sara Reardon is a freelance science reporter based in Bozeman, Montana. She is a former staff reporter at Nature, New Scientist and Science, and has a master’s degree in molecular biology. www.sarareardon.com, Twitter @sara_reardon.
Source: Read Full Article