“Symptoms, then, are in reality nothing but a cry from suffering organs” – Jean-Martin Charcot
Nearly 130 years after his death, Jean-Martin Charcot’s name still resonates with modern neurologists. The famed 19th century French physician made myriad enduring contributions to the field. His eponymous foot condition might be his best known. He also delved into neurosyphilis, multiple sclerosis, and amyotrophic lateral sclerosis (or Charcot disease, as it’s called in France). A genetic disorder that causes damage to the peripheral nerves bears his name too (Charcot-Marie-Tooth disease).
Working from a pathological perspective — for he was, first of all, a pathologist — Charcot honed in on these cardinal neurological conditions, separating them from the all-encompassing diagnosis of “hysteria” by reviving and systematizing what was called the anatomo-clinical method, while also contributing to the development of the neurologic exam.
Portrait of French neurologist Jean-Martin Charcot c. 1890.
A pioneer in incorporating microscopy and photography into medicine, the avant-garde technologies of his era, Charcot also mentored trainees the likes of Charles Babinski, Gilles de la Tourette, and Sigmund Freud — clinicians who would make a fairly substantial splash.
But Charcot also had his warts.
Growing into the quintessential celebrity doctor of the 19th century, he ventured into the testing of various, not-so-benign, chemical and physical phenomena and into the non-neurological realm of the “hysterical” conditions, approaching it with theatrics, hypnosis, and perhaps even some rehearsed patient performances. But he was, after all, a product of an era when medicine was just beginning to distinguish itself from a plethora of magical beliefs that permeated society. And to this day he remains an integral figure in understanding disorders afflicting the brain and nervous system.
Far Exceeding Modest Expectations
Born November 29, 1825 in Paris, Jean-Martin Charcot had to compete to obtain a university education. His father, Simon-Pierre Charcot, was a maker of carriages, shoes, and cabinets who could afford to have only one of his four sons educated. Outperforming his three younger brothers in school, Jean-Martin was a gifted artist but also drawn to medicine, ultimately choosing to study the latter at the University of Paris.
Graduating from medical school as an average student in 1853, Charcot was able to secure an internship at the Pitié-Salpêtrière. Though affiliated with the esteemed Sorbonne University, the Salpêtrière had a rather mediocre reputation. Built as a weapons factory and gunpowder storage site to serve King Louis XIII (reign, 1610-1643), the facility had been converted into an asylum by his successor Louis XIV (reign, 1643-1715).
The Salpêtrière Hospital, depicted in the late 1800s.
Notorious in the mid-18th century as a place where the insane, destitute, and hopelessly ill were admitted with little hope of being released, Charcot described the Salpêtrière as the “grand asylum of human misery.” But he considered the institution’s 5000 patients a virtual pathological museum from which he and others could come to understand disease.
Many patients at the Salpêtrière were designated as suffering from “hysteria.” This was the default diagnosis for anyone exhibiting any “symptoms” or “signs” that might at least remotely relate to the nervous system: headaches, deafness, psychosis, anxiety, homosexuality, and even women acting independently in matters of politics and religion.
Though dissected by anatomists since antiquity, the central nervous system was still terra incognita at the time of Charcot’s internship. The very scientist who would prove the CNS to be comprised of cells, Spanish neuroscientist Santiago Ramón y Cajal, was barely a toddler and the idea of the spinal cord being an extension of the brain was just a hypothesis.
Art Becomes Science
Delineating several conditions of the first category is how Charcot would earn his legacy, creating what we now know as neurology. He thrived during his internship, and under the influence of his medical school dean, Dr Pierre-François Rayer (1793-1867) — a pathology professor who also attended to the health of Emperor Napoleon III — decided to study pathology. He excelled partly because this was an era before pathologists regularly photographed and reliably preserved specimens: Charcot’s artistic ability came in handy when documenting anatomy.
In 1857, the Salpêtrière appointed Charcot professor of medicine, and subsequently chief of medical services. But Charcot’s patient care work melded with his pathological perspective. Along with Rayer, Charcot’s mentors included Guillaume Duchenne (for whom Duchenne muscular dystrophy is named). Duchenne provided pathological specimens to Charcot and introduced him to neurological examination, as well as the utilization of photography in medicine.
Charcot also found a mentor in the pathologist Alfred Vulpian (1826-1887), who taught him microscopy; it was a technology invented in the 17th century but was just then coming of age for the examination of histological specimens.
During the mid-19th century, histology was particularly challenging on nervous tissue. To be sure, the Czech anatomist Johannes Purkinje (1787-1869) had demonstrated the presence of what we now call neurons in the cerebellum as early as 1837. However, the real advances would come later in the century with ascent of Ramón y Cajal and Camillo Golgi (1843-1926) of Italy.
In debating between Golgi’s idea that the CNS was a continuous electrical network and the Cajalian idea that it was composed of cells, the two scientists would introduce a new staining technique (invented by Golgi and improved by Ramón y Cajal) that would earn them both the 1906 Nobel Prize in Physiology or Medicine. Using potassium dichromate and silver nitrate, the technique would darken myelinated axons, dendrites and neurofibrils, while leaving other entities lighter, thereby elucidating the CNS tracts and nuclei beginning around the midpoint of Charcot’s career.
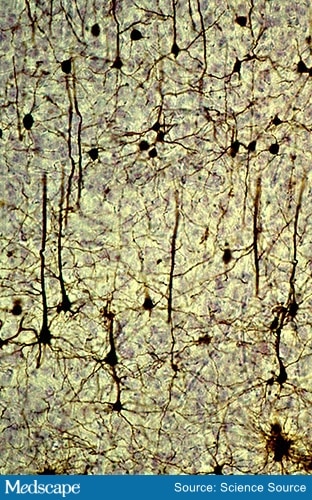
An example of the Golgi-Cajal staining method
Previously, pathologists could see the boundaries between gray and white matter, but much less distinctly. Cutting carefully through the spinal column in cross sections, they could make out a certain degree of spinal cord anatomy. By the 1860s, Charcot was doing this too, and while he may not have been the first to see the spinal cord in this way, he was the first to connect what he was seeing with particular neurologic manifestations.
Autopsies Worthy of Enthusiasm
The anatomo-clinical method involved correlating autopsy findings with clinical manifestations recorded prior to each patient’s death. Charcot was reputed for anticipating postmortem findings in advance, with plenty of enthusiasm. One such case was that of a maid working in Charcot’s house who was dropping dishes with increasing frequency. The head maid wanted her fired, but Charcot kept her working, hoping to observe her decline and perhaps, eventually, perform an autopsy. “Many dinner sets later,” in the words of neurodegenerative disease researcher and comedian Dr Aaron Wagen, “Charcot diagnosed MS.”
Postmortem work by Charcot in similar patients revealed sclerosis — or stiffened nervous tissue replaced by connective tissue. What’s more, these sclerotic lesions occurred at more than one location, hence he included the word multiple in his newly christened diagnosis.
Whereas MS could include some mental impairment and take a fairly chronic course, waxing and waning over many years, Charcot was also noticing patients afflicted by muscle impairment that tended to spare mental processes, but progressed faster to paralysis and often death within a few years. Presenting to Charcot in 1865, one such patient named Marie suffered progressive paralysis and contractures beginning in her arms, followed by her legs, and consequently had been deemed “hysterical,” despite the lack of mental impairment. Eventually, her breathing muscles were affected and she died.
Working with one of his trainees, Dr Alix Joffroy (1844-1908), Charcot autopsied Marie and other patients with similar histories over the next several years. Autopsy showed lesions in the lateral part of the spinal cord, where motor impulses are transmitted to the limbs via the lateral corticospinal tract. The lesions were sclerotic, leading to progressive muscle wasting, or amyotrophy. As many of the lesions were in the lateral column, in 1874 Charcot coined the term amyotrophic lateral sclerosis.
From Questionable Clinician to Celebrity Doc
Charcot’s work was clearly foundational for the diagnostic end of neurology, but things get messy when we look at his therapeutic endeavors. He liberally gave mercury to patients with syphilis, rubbing it all over their bodies. He also prescribed ergot alkaloid-containing rye and hot iron cauterization to the back — both, like mercury, known to dangerous by that time — as well as agents with doubtful efficacy, such as zinc sulfate and silver nitrate.
To be sure, some treatments he advocated were known to provide benefit, like bromides for epilepsy. For various conditions, Charcot also tried hydrotherapy (shooting cold water at patients from a high-pressure hose) and electrotherapy (shocking various body parts). Perhaps the shocking helped him to elucidate anatomic connections with various nerves and muscles, aiding his contributions to the neurologic exam, but it couldn’t have been pleasant for the patients.
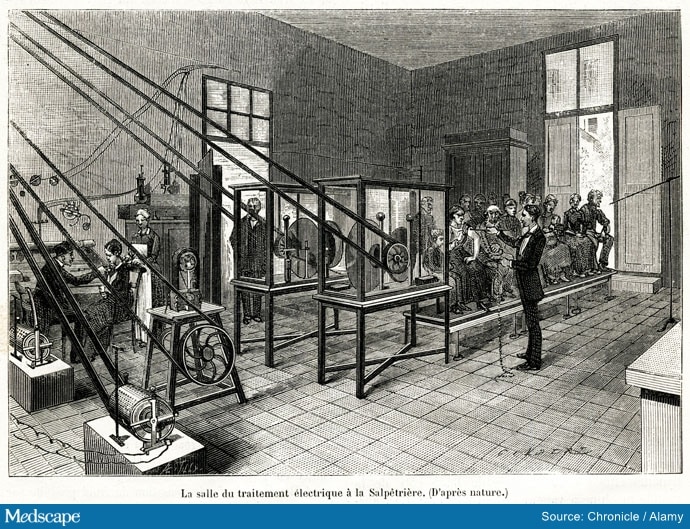
The neurologist Jean-Martin Charcot in a consulting room of the mental hospital Pitié-Salpêtrière Hospital in Paris. Patients wait for treatment with an electric current.
Yet Charcot would go on to become a celebrity doctor, perhaps partly from his success in delineating ALS, MS, and neurosyphilis, as well as peripheral neurological conditions like Charcot foot and Charcot-Marie-Tooth disease.
Furthermore, much like pioneering neurosurgeon and endocrine scientist, Dr Harvey Cushing, Charcot’s contributions extended beyond just his own field. Consider the triad consisting of right upper quadrant pain, jaundice, and fever, suggesting acute cholangitis. To this day it’s called the Charcot triad.
Another booster for Charcot’s celebrity status were his public lectures. Offered mostly on Tuesday mornings, the lectures could be rather theatrical, as in one instance when Charcot attached a baguette to a patient’s head to make a head tremor more obvious to the audience.
Later in his career Charcot turned his attention to conditions presenting with not only neurologic signs, but those with symptoms connected to personality and behavior. And to his credit, he rejected the idea of “hysteria” as causing such conditions. He insisted that pathology underlying any behavior must lie in the brain itself.
But he did nevertheless conflate some cases of epilepsy with “hysteria.” To manage such patients and demonstrate their conditions to the public, he once again embraced dramatic procedures, like hypnosis and electrostimulation. He demonstrated hypnosis as a means for triggering convulsions and other “hysterical” phenomena, presenting patients in front of live audiences. One such patient was Marie “Blanche” Wittmann (1859-1913). Not to be confused with Marie the ALS patient, Wittmann was called the “Queen of Hysterics,” because she could be triggered to convulse through hypnosis; that is, until Charcot’s death at the age of 67 (some suspect he’d convinced her to “act”).
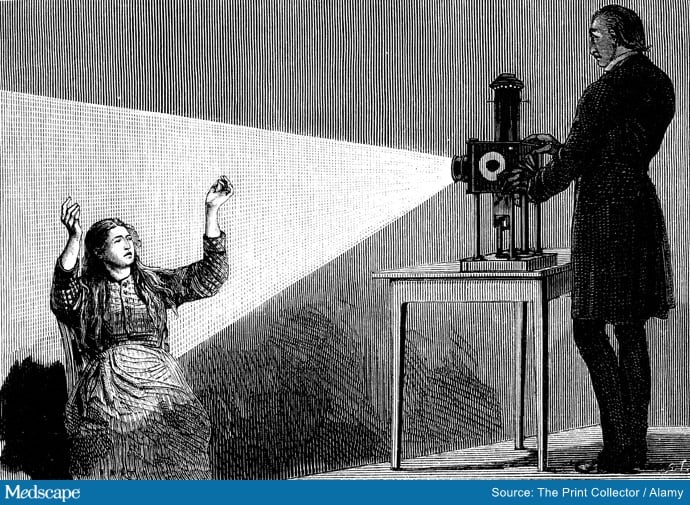
Jean-Martin Charcot demonstrating hypnosis, 1879.
Charcot wound up living the celebrity life. He mingled among 19th century Parisian upper society and indulged copiously in the poor health habits that came with doing so. Wine. Smoking. Rich, fatty foods.
He died of heart failure on August 16, 1893, after which Marie, Queen of Hysterics, outlived him by two decades, never suffering another hysterical episode again.
Dr Warmflash is a freelance health and science writer living in Portland, Oregon. His recent book, Moon: An Illustrated History: From Ancient Myths to the Colonies of Tomorrow, tells the story of the Moon’s role in a plethora of historical events, from the origin of life, to early calendar systems, to the emergence of science and technology, to the dawn of the Space Age.
For more news, follow Medscape on Facebook, Twitter, Instagram, and YouTube.
Source: Read Full Article