Depression is a leading cause of disability worldwide, with middle-aged and older adults disproportionately affected, a global demographic that is quickly expanding.
To better understand the reasons behind how this age group develops depressive disorder, commonly referred to as depression, Stephen Aichele, assistant professor in the Colorado State University Department of Human Development and Family Studies, and his team used a machine learning approach to analyze data from a large, population-representative sample of middle-aged and older European adults.
It is one of very few studies to use such an approach for comparing numerous risk and protective factors for depression in later life, and it is likely the first to apply it so broadly within this population (with 18 European countries represented and 56 risk and protective factors examined).
Risk factors for depression
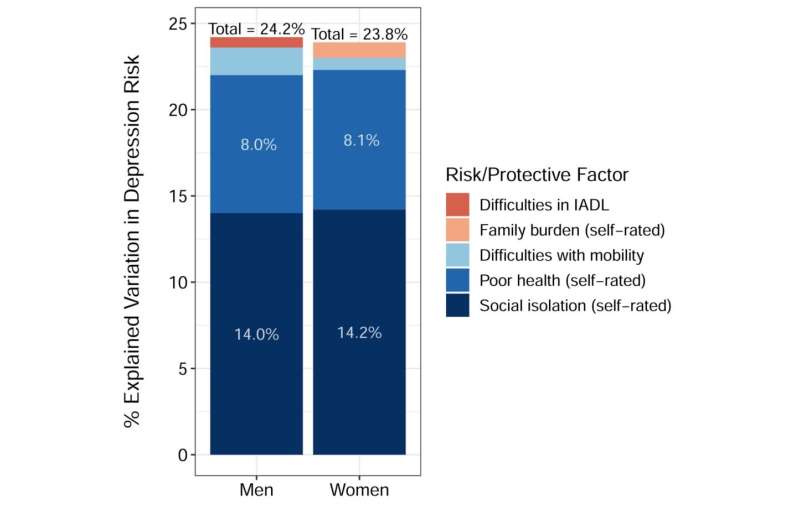
Out of 56 variables examined, Aichele and his team found that, for both men and women, social isolation was the primary risk factor for depression, followed by general poor health and mobility difficulties.
Other recent studies have identified social isolation as a key risk factor for depression in older adults, but Aichele and his team also looked at 30 variables related to specific dimensions of participants’ social networks and family configurations, such as frequency of contact, number of friends, and interpersonal transactions related to physical care and financial support.
“It’s less about frequency of contact or how many friends you have,” said Aichele. “It’s more about physical proximity to the person you feel emotionally closest to, be it your spouse, partner, or other primary social relation.”
For men, a fourth key risk factor was difficulty in instrumental activities of daily life, such as managing finances, taking medications and making telephone calls. For women, a fourth key risk factor was family burden—women who strongly agreed that “family responsibilities get in the way of my being able to do the things I want to do” were at elevated risk for depression. However, these gender-specific factors accounted for only a small proportion of differences in depression risk.
“Depression prevalence in older women is about twice as high as in older men,” said Aichele. “And yet, the same primary risk factors show up for both (social isolation, poor health, mobility problems). The reason for that discrepancy has not been solved, at least by this study.”
Cognition and health analytics
Research in Aichele’s lab centers on the use of advanced statistical approaches to understand age- and disease-related changes in cognition and mental health following middle age. Aichele’s first published study to use machine learning showed that age-related decline in older adults’ information processing speed was closely linked to mortality risk—comparable in its predictive effect to knowing a person’s tobacco smoking history.
More recently, Aichele and colleagues used “bivariate latent change score models”, a type of time series analysis, to show that lower memory and problem-solving performance at a given age reliably precedes two to three year increases in depressive symptoms in older adults.
“If we can detect cognitive decline early enough, there may be a window of time to prevent related increases in depression risk,” said Aichele. “It’s then a matter of figuring out what factors exacerbate or mitigate the effects of cognitive loss on depression.”
As a step toward that aim, Aichele and his team again used a machine learning approach, random forest analysis (RFA), to compare risk and protective factors for depression using data from the Survey of Health, Ageing and Retirement in Europe (SHARE). Study participants ranged in age from 45 to 105 years and represented 18 European countries. SHARE data spans a wide array of sociodemographic, health-related, economic, and cognitive variables. Importantly, SHARE also includes multiple measures of participants’ relational networks.
“We wanted to target a wide variety of risk and protective factors for depression,” said Aichele. “And we felt it would be especially important to look at different dimensions of social and relational support given that self-reported social isolation may be more closely linked to some factors than others.”
The RFA methodology was chosen for the analyses because it considers potentially complex interactions between risk factors (for example, between memory problems and quality of social interactions) in rankings of risk factor importance.
“Conventional statistical approaches are poorly suited for comprehensively testing such complex associations,” said Aichele.
Source: Read Full Article