Scientists have shown it is possible to reverse a key process that allows pancreatic cancer cells to grow and spread around the body.
These findings, published in Nature, show that a protein called GREM1 is key to regulating the type of cells found in pancreatic cancer—and manipulating its levels can both fuel and reverse the ability of these cells to change into a more aggressive subtype.
The researchers believe this fundamental discovery could ultimately pave the way for new pancreatic cancer treatments.
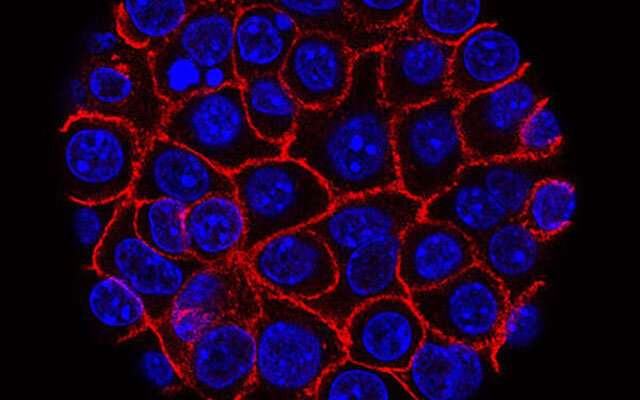
Researchers from The Institute of Cancer Research, London, studied pancreatic cancer with the gene that makes the GREM1 protein switched off in mice, and in pancreatic “mini-tumors,” which are also known as organoids.
Switching off GREM1 caused the tumor cells to rapidly change shape and develop new properties that help them invade new tissues and migrate around the body. Within just 10 days, all the tumor cells changed their identity into a dangerous, invasive cell type.
Switching off the gene also made tumors in mice more likely to spread. The researchers studied a mouse model of pancreatic ductal adenocarcinoma (PDAC)—the most common and aggressive form of the disease. Around 90 percent of mice without functioning GREM1 developed tumors which had spread to their liver, compared to 15 percent of mice where GREM1 was working normally.
Crucially, the scientists, who were largely funded by The Institute of Cancer Research (ICR), which as well as being a research institute is also a charity, then showed that boosting GREM1 levels could reverse this process and cause invasive cell types to revert into a less dangerous form. Researchers hope, in the future, to use this knowledge to find ways to reverse more advanced pancreatic cancer into a less aggressive form, which is easier to treat.
The researchers, who work in the Breast Cancer Now Toby Robins Research Centre at the ICR, stress that the science is early stage, and significant amounts of research would be required to discover and develop treatments that change PDAC cell fates and make the tumor respond better to therapies. However, fundamental discoveries such as this are crucial in directing efforts to find new cancer drugs and treatments.
Pancreatic cancer has the lowest survival rates of common cancers. Less than seven percent of people will survive for five years or more. More than 10,000 people are diagnosed with pancreatic cancer in the UK each year, and more than 9,000 will die from it.
The researchers also discovered that another protein, called BMP2, is involved in regulating GREM1, and that these two proteins regulate the form PDAC cells ultimately take, according to a mathematical model first proposed by Alan Turing in 1952. These “Turing patterns” are found in nature—from the patterns on the skin of the giant puffer fish to seashells—and strikingly the same sort of patterns are seen in the different types of cells found in pancreatic cancer. Further studies are needed to determine whether this model is also applicable in other forms of cancer.
Professor Axel Behrens, leader of the Cancer Stem Cell Team at the Institute of Cancer Research, London, and senior author of the study, says that “this is an important and fundamental discovery that opens up a new avenue for uncovering treatments for pancreatic cancer. We have shown that it is possible to reverse cell fate in pancreatic cancer in the lab—turning back the clock on aggressive tumors and switching them to a state that makes them easier to treat. By better understanding what drives the aggressive spread of pancreatic cancer, we hope to now exploit this knowledge and identify ways to make pancreatic cancer less aggressive, and more treatable.”
Source: Read Full Article