Editor’s note: Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
Scientists and lawmakers agree that over-the-counter covid tests could allow desk workers to settle back into their cubicles and make it easier to reopen schools and travel.
But even as entrepreneurs race their products to market, armed with millions of dollars in venture capital and government investment, the demand for covid testing has waned. Manufacturing and bureaucratic delays have also kept rapid tests from hitting store shelves in large numbers, though the industry was energized by the Food and Drug Administration’s greenlighting of two more over-the-counter tests Wednesday.
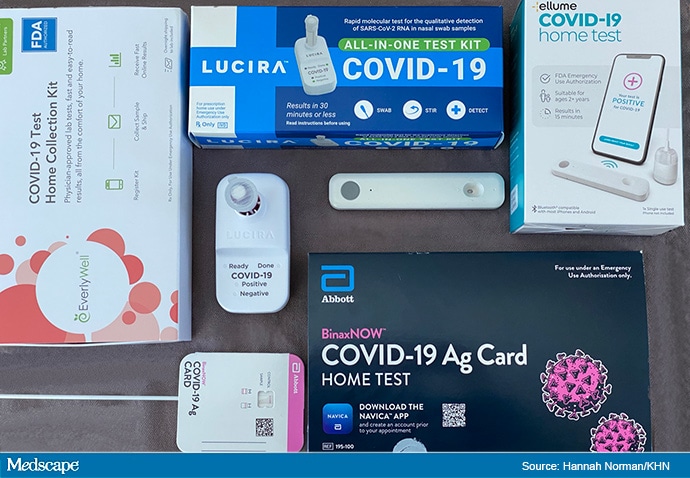
Corporate giants and startups alike plan to offer a dizzying array of test options, most costing between $10 and $110. Their screening accuracy varies, as does the way consumers get results: collection kits mailed back to a lab, devices synced with artificial intelligence-enabled apps on a smartphone that spit out results within 15 minutes, and credit card-sized tests with strips of paper that must be dipped into a chemical substance.
“At-home tests are one of the key steps to getting back to normal life,” said Andy Slavitt, a member of the White House COVID-19 Response Team, during a February briefing.
The Biden administration announced in March it will allocate $10 billion from the recently passed stimulus package for covid testing to expedite school reopenings, and earlier said it would invoke the Defense Production Act to manufacture more at-home tests. Separately, the federal government has already sent millions of Abbott Laboratories’ BinaxNOW rapid tests to states, and California, for instance, is giving 3 million of them to its most disadvantaged school districts for free.
Large employers, like Google, sports leagues and the federal government, have already shelled out millions to regularly test their workers. Amazon just received emergency use authorization from the FDA for its own covid test and home collection kit, which it intends to use for its employee screening program.
Individuals who want to buy over-the-counter tests can bill their health insurance plans, which are required by the federal government in most cases to fully cover covid tests that have been authorized by the FDA.
Everlywell, based in Austin, Texas, is an at-home diagnostic company that already sells its collection kit to consumers through its website and Walgreens, and will soon offer same-day delivery via DoorDash in a dozen cities. Dr. Marisa Cruz, Everlywell’s executive vice president of regulatory and clinical affairs, said buyers can seek reimbursement from their insurance plans for the kit’s $109 cost. The tests are also eligible for purchase with pretax dollars from health savings or flexible spending accounts, she said.
Even with vaccines, epidemiologists say, rapid tests are desperately needed because more testing, along with mask-wearing and physical distancing, will get people back in offices and classrooms and help catch cases that go undetected. A report by the Centers for Disease Control and Prevention found that, of people with active infections, 44% reported no symptoms.
But the market for over-the-counter tests is risky. Demand for testing has plunged dramatically since the height of the winter surge and may not rebound as more people are vaccinated.
“You clearly are at risk of missing the market,” said Michael Greeley, co-founder and general partner at Flare Capital Partners, a venture capital firm focused on health care technology.
But Douglas Bryant, president and CEO of Quidel Corp., remains unfazed, even after the diagnostics manufacturer’s testing demand dropped by about one-third in the past two months.
“The level of testing for people with symptoms and the ‘worried well,’ who see others getting tested and think they should, too, is subsiding,” Bryant said. “But once we start to get more people vaccinated, the government will move from campaigning to get people vaccinated to saying, ‘Please test yourself regularly so we can get back to work.'”
Quidel, headquartered in San Diego, recently unveiled its latest test, the QuickVue A t-Home COVID-19 Test, which takes 10 minutes to detect the coronavirus by homing in on specific proteins, called antigens. The FDA authorized the test for over-the-counter use Wednesday, and Quidel plans to announce retail partners in the coming weeks.
The FDA said in mid-March it would speed the pipeline for “screening testing,” including at-home covid tests that don’t require consumers to have symptoms or a prescription.
In February, the Biden administration cut a $232 million deal with Ellume, whose rapid antigen test was authorized by the FDA in December. Paired with an app, the test takes 15 minutes to analyze after a nose swab.
The Australian company currently ships hundreds of thousands of test kits a week to the U.S. from its factory in Brisbane to large companies and the Department of Defense. It plans to be on the shelves of multiple pharmacies by the second half of the year and in one major retailer in April, said Dr. Sean Parsons, the company’s founder and CEO.
“We are going as fast as we can possibly go,” he said.
The main holdup for Ellume has been getting enough swabs for its production line. The company is building a factory in the U.S. to reduce international shipping costs and increase production.
Abbott, which dominates the rapid-test market, said in January it expects to sell 120 million BinaxNOW antigen tests to consumers in the first half of the year. People who take the test now must do so under observation by telemedicine platform eMed. But Abbott received authorization from the FDA this week for an over-the-counter version that won’t require remote observation or a prescription. The test will be available in U.S. stores in the coming weeks, the company said.
Throughout the pandemic, the government has depended heavily on medical device behemoth Abbott’s testing options. The company’s rapid-diagnostics arm alone has snared $673 million in federal contracts to combat the coronavirus, according to a ProPublica database. This includes bulk purchases made by the Defense Department, the national prison system, Immigration and Customs Enforcement, the State Department and former President Donald Trump’s office.
But antigen tests sometimes report false negatives, particularly among people without symptoms, noted Dr. Jac Dinnes, who co-authored a review of 64 covid test studies. By comparison, polymerase chain reaction (PCR) tests — generally employed by commercial labs — are more sensitive. PCR tests search for the virus’s genetic material over multiple testing cycles, which magnifies what’s in the swab sample, requiring a much smaller viral load for detection.
Antigen tests are the basis for most at-home screening, but the FDA has also authorized two at-home options — made by Lucira Health and Cue Health — that use molecular processes similar to a PCR test.
Still, many experts support the widespread distribution of cheap, rapid tests, even if they aren’t as sensitive as lab-run alternatives, and see a demand. In Germany, the supermarket chain Aldi began selling rapid tests in early March, roughly $30 for a five-pack, and sold out within hours. One recent study found that if a pack of tests was mailed to every household in the U.S. — even assuming that up to 75% would go into the garbage — they would save thousands of lives and avert millions of infections.
“Don’t let perfect be the enemy of good,” said study co-author and Yale University professor A. David Paltiel. “This doesn’t have to work perfectly to make a huge difference.”
Some companies are working on rapid-testing options that more precisely read samples, such as Gauss.
The Menlo Park, California, health tech company, which before the pandemic created an artificial intelligence-based app to measure surgical blood loss in real time, aims to harness its expertise to improve on the basic antigen test. It took about a week for CEO Siddarth Satish to raise $30 million of venture capital last October.
Its covid-testing app uses facial recognition software to confirm that test-takers correctly swab their noses. The app provides step-by-step instructions and timers. After 15 minutes, an algorithm based on thousands of sample tests interprets the result — which displays as a colored line, as with a pregnancy test — using the phone’s camera.
Gauss and Cellex, which manufactures the Gauss tests, await FDA authorization. In the meantime, they have produced more than 1.5 million kits and struck deals with supermarket chain Kroger and e-pharmacy site Truepill to sell them for about $30.
“A huge part of the accuracy issue with rapid tests is that you have to visually interpret them,” Satish said. “Sometimes you get really faint lines, just like with a pregnancy strip, and there’s some guesswork.”
Lucira Health, based in Emeryville, California, uses something called loop-mediated isothermal amplification technology, which is similar to PCR tests in precision. In February, the company went public, raising $153 million largely to fund the manufacturing of its all-in-one testing kit, currently prescribed by doctors across the country. The kit comes with a nose swab and a vial of chemicals analyzed by a hand-held device — taking up to 30 minutes for results.
Kelly Lewis Brezoczky, Lucira’s executive vice president, envisions the test kit on the shelf in local pharmacies, perched next to the NyQuil. “I always like to tell people that it is as easy to use as toothpaste,” she said.
Source: Read Full Article