The gene editing technique CRISPR has been making headlines worldwide for its potential to change the genetic makeup of organisms and treat genetic diseases such as sickle cell anemia. It has vast potential in many areas—including neuroscience.
“Neuroscientists are currently using this technique to unravel how the brain works and hope to one day adapt it to offer treatments and cures for various neurological disorders, with certain forms of blindness perhaps most imminent,” said Kate O’Connor-Giles, Provost’s Associate Professor of Brain Science at Brown University. “The possibilities for neuroscience are wide open.”
CRISPR allows researchers to precisely cut and alter the DNA of a cell. Using CRISPR, scientists can probe the genes that underlie nervous system function in model organisms by introducing mutations, including those associated with disease. This allows scientists to study the effects of changes in genes on nervous system development, function and behavior.
CRISPR consists of two components: Cas9, an enzyme that cuts DNA and is often referred to as molecular scissors, and a synthetic RNA molecule called a gRNA, which can be programmed to recognize specific sites in the genome.
“You can target Cas9 pretty much anywhere in the genome where it will then cleave DNA,” said O’Connor-Giles, who is affiliated with Brown’s Carney Institute for Brain Science. “This then opens a window of opportunity for re-coding the DNA by hijacking the cell’s DNA repair machinery. This allows us to do all sorts of things, such as deleting one or more genes or introducing different kinds of mutations.”
O’Connor-Giles discussed how she and her team have been using the CRISPR technique, as well as what neuroscientists like her hope to do in the future, ahead of an April 27 Carney Conversations event where she’ll further explore the potential of gene editing technology in neuroscience.
Q: Why is CRISPR important for neuroscience?
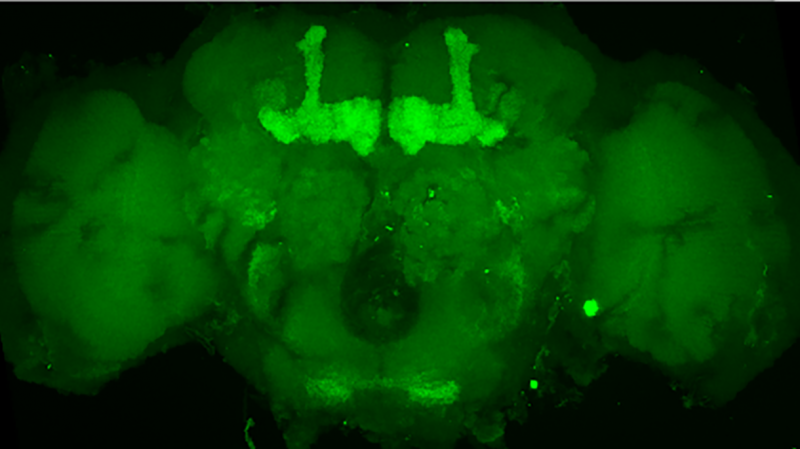
Many of the genes that regulate nervous system development, function and maintenance are poorly understood. Changing this is one of the major areas of research in our lab. With it becoming easier to determine what genetic changes lead to atypical neurodevelopment, many uncharacterized genes are being linked to neurological disorders. CRISPR allows us to rapidly generate animal models to study how these genes function in an intact nervous system.
Similarly, CRISPR can be used for studying gene mutations in human cells. Neurons can be induced from stem cells with the altered gene, as well as from stem cells in which the disease-causing change has been repaired by CRISPR. This allows neuroscientists to study the effect of disease-associated genetic changes in the exact genetic background of the person to understand how that change is impairing the nervous system in the specific context of that person’s neurons. This is important because we all have slightly different genomes with small changes sprinkled throughout that may alter the effect of a disease-associated change.
In combination, animal and stem cell models generated with CRISPR technology are powerful tools for understanding neurological disorders. We can use CRISPR to study the effect of differences in genes on brain aging. We can also use CRISPR in model organisms to identify new genes that play important roles in the nervous system. The more of this we achieve, the more likely it is that when a change in a gene is found to underlie a neurological disorder in a patient, we’ll already have an understanding of what that gene does and what treatment options may be available, or promising avenues for investigation.
Q: When did you first hear about CRISPR and realize that you wanted to incorporate it into your research?
In 2012, my lab wanted to use gene editing to study new genes we had identified as candidate regulators of communication in the brain. We started by working to improve methods for gene editing in flies, which back then was time-consuming and often not even possible.
We were following any developments in gene editing closely, and we started paying attention to CRISPR as soon as the Doudna and Charpentier labs showed that it could be used to edit DNA in a tube. When multiple labs showed in January and February 2013 that CRISPR could work in cells, it was instantly clear that this approach was as simple as the first step in gene editing—cutting DNA at a specific site—was going to get. So, we decided to immediately focus our efforts on adapting CRISPR in flies and formed a collaboration with the labs of Jill Wildonger and Melissa Harrison. We had our first evidence that CRISPR was working in flies by April 2013, and we published the results the following month. This gave us the ability to essentially edit genes at will in flies, and we prioritized the open distribution of our reagents and approaches to make sure this was true for the entire fly community. It was a pretty exciting time, and I’m thrilled to have been part of it. The impact has been long-lasting, with CRISPR completely revolutionizing our ability to study neuronal genes in the lab.
Q: How do you see CRISPR impacting the treatment and cure of brain disease?
CRISPR greatly expands our ability to study disease mechanisms in model organisms and stem cells so that we can understand why neurological function is negatively affected. This foundational research is currently the area where CRISPR has the greatest impact. In our lab, for example, we’re using CRISPR to study genes whose loss has been linked to intellectual disability but have not been studied in the context of the brain. While there is also potential to use CRISPR to cure neurological disease, this needs to be balanced against the risks associated with breaking DNA. The delivery of CRISPR components to cells in the brain also presents a challenge. For this reason, retinal disorders involving more accessible neurons in the eye are currently the most promising candidates for CRISPR-based treatments in the nervous system.
Q: What are some of the challenges associated with using CRISPR to manipulate genetic materials in humans?
I think there are three primary concerns when considering manipulating human genomes. First, safety—can we use CRISPR in a way that doesn’t risk introducing mutations? Breaking DNA is inherently risky. The cell won’t necessarily repair the break as planned, and we could break DNA at unintended sites in the genome, accidentally introducing new mutations that could disrupt the function of other genes and result in different deleterious effects depending on the affected gene or genes.
Second, efficacy—can we actually conduct CRISPR in humans with high enough efficiency to be useful in the treatment of disease? As I mentioned, a major bottleneck here is the delivery of CRISPR components to the relevant cells. This is especially true in the human nervous system with its billions of neurons.
And third, there are ethical concerns, for example, surrounding equitable access to CRISPR-based therapies and the use of CRISPR to make changes to genomes that go beyond correcting disease-associated changes. This is a critical issue that extends well beyond the science, and should involve all of us thinking hard about how we do and do not want to use gene editing in humans. This is one of the main reasons it’s so important that we all have a basic understanding of CRISPR, what it can and can’t do, and how this may change in the relatively near future.
Q: How is the technology as a research tool changing, and what are ways it can be improved?
Source: Read Full Article