
At least 60 people have now died in the current New South Wales COVID outbreak.
We’ve been keeping track of how old these people were, and have observed 85% of the COVID deaths up to August 18 (51 out of 60) were among people aged over 60.
We’ve also been taking note of reports on their vaccination status. It appears 96% of those over 60 who have died (49 of 51) were not vaccinated, or had only received one dose.
These deaths are tragic and, in all likelihood, were preventable. So if you’re over 60 and are yet to be vaccinated, now is not the time to hesitate.
Older age increases your risk from COVID-19
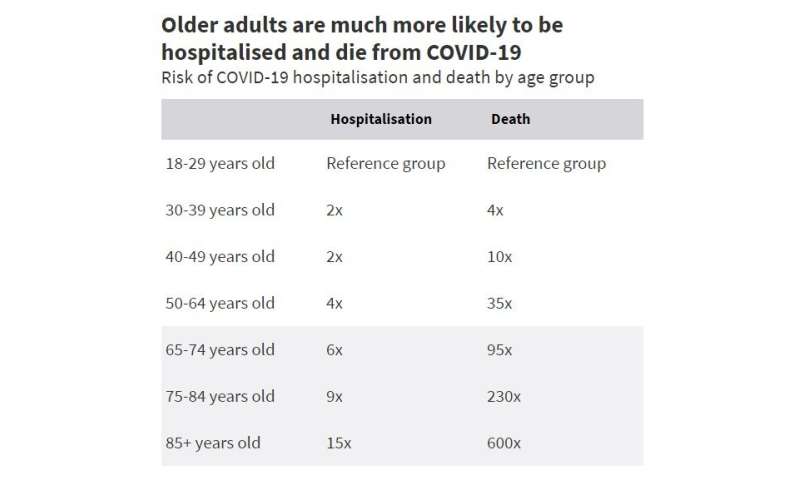
Age is a major risk factor for serious illness and death from COVID-19.
A person aged 65-74 is at six times greater risk of hospitalization and 95 times greater risk of dying compared to an adult under 30.
People over 85 are 15 times more likely to be hospitalized and 600 times more likely to die than 18 to 29-year-olds.
This is why Australia’s vaccination program has prioritized older adults.
So why do people in this age group remain unvaccinated?
Most older Australians are vaccinated
It’s important to acknowledge that of the 5,632,555 Australians aged 60+, more than 4.4 million (79%) have had a first dose of a COVID-19 vaccine.
This ranges from 71% for 60 to 64-year-olds, to 86% for 75 to 79-year-olds.
So despite the criticism of Australia’s vaccination program, more than three-quarters of Australians aged 60+ have at least partial protection from COVID-19.
Still, that leaves 1.2 million Australians aged 60+ yet to receive a first dose of any COVID vaccine, despite having been eligible for vaccination for several months.
What are they waiting for?
For a variety of reasons, no vaccine ever achieves 100% take-up. But most Australians over 60 want to be vaccinated. Surveys have shown over 65s are the least hesitant age group. As of August 7, only 6.75% of adults over 65 were unwilling to be vaccinated.
Some people have experienced difficulty accessing the vaccine. In particular, we need to improve access in areas which are more vulnerable to COVID outbreaks.
But according to data from the Australian Bureau of Statistics published last month, around 25% of unvaccinated people over 70 are waiting for a different vaccine option.
We can read this to mean they’re waiting for what they perceive to be a “better” vaccine—an mRNA vaccine from Pfizer or Moderna.
Sadly, with the NSW outbreak escalating, and the increasing frequency and likelihood of COVID outbreaks across Australia, some of these folks may die waiting.
AstraZeneca is a highly effective vaccine
The vaccine for which all people aged 60+ in Australia are currently eligible is AstraZeneca.
While adequate supply of the Pfizer vaccine has been an ongoing issue and shipments of the Moderna vaccine are yet to commence, AstraZeneca is being produced in Australia and is widely available.
But not everyone is keen on it.
Some of the lack of enthusiasm surrounding the AstraZeneca vaccine relates to the perception it is less effective than Pfizer.
The most important outcome, however, is prevention of serious illness from COVID-19, and both vaccines perform similarly well on this metric after two doses. Recent modeling from the Doherty Institute assumed an 86% reduction in hospitalization with the Delta variant after two doses of AstraZeneca, compared to 87% after two doses of Pfizer.
For deaths from Delta, the difference is also very small. The AstraZeneca vaccine is believed to achieve a 90% reduction after two doses, compared to 92% with Pfizer.
Although milder COVID-19 infections occur more commonly in people who have been fully-vaccinated with AstraZeneca, “breakthrough” infections also occur with Pfizer.
So, the benefits of AstraZeneca are clear and the differences between AstraZeneca and Pfizer in terms of effectiveness against the most worrisome outcomes of COVID-19 are very small.
But what about the risks?
Both vaccines have common side effects including pain at the injection site, fatigue and headache. While these side effects are more common with AstraZeneca, they don’t last long with either vaccine.
So that brings us to blood clots. In March, just weeks into the launch of Australia’s vaccination program, reports emerged of a rare clotting syndrome following use of the AstraZeneca vaccine.
Named thrombosis with thrombocytopenia syndrome (TTS) to describe the unusual combination of serious blood clots with a low platelet count, the discovery of this significant complication saw changes to COVID-19 vaccination guidelines in many countries, including Australia.
Deaths from TTS have received extensive coverage in the media, and concern about this condition is undoubtedly a key reason for reluctance towards AstraZeneca.
But importantly, the risk of TTS is small, and becomes lower as you get older (the opposite of the risk from COVID-19). The Australian Technical Advisory Group on Immunisation has estimated below age 60, the incidence of TTS is 2.7 per 100,000 doses. Over age 60 the incidence is thought to be 1.8 in every 100,000 doses.
Of 112 cases of confirmed or probable TTS that have occurred in Australia to date, a total of six people have died. One was over 60 (a 72-year-old woman).
Based on these statistics, if the 1.2 million Australians over 60 not yet vaccinated all received AstraZeneca, we would expect about 22 to develop TTS and one or two of them to die.
While these are serious albeit rare complications, remember that in NSW, in an outbreak with close to 10,000 cases of COVID-19 diagnosed to date, more than 50 people over 60 have already died and more will unfortunately follow.
Balancing the risks and the benefits
Balancing risks and benefits is key to informed decision-making before taking any medication; none are risk-free.
For those 1.2 million Australians over 60 yet to be vaccinated, the benefits of taking the vaccine available now—AstraZeneca—are high, and for most people will outweigh the small risks.
The threat of COVID-19 is no longer theoretical, especially for those living in Sydney and other major metropolitan cities.
Source: Read Full Article