A new study provides insights into the curative effects of gluten-free diets in celiac patients. Results from the proteomics-based research suggests not.
celiac disease is a highly prevalent disorder characterized by a harmful immune reaction to dietary gluten proteins in the upper small intestine. The disease is caused when CD4+ T-cells in a patient respond to gluten, mounting an immune reaction that causes intestinal damage.
Tracking celiac disease: intestinal biopsies
Disease diagnosis and monitoring are typically performed via expert analysis of intestinal biopsies by medical professionals. The only current effective treatment for celiac disease is complete and permanent removal of gluten from patients’ diets. For the vast majority of patients, biopsies reveal that avoiding gluten in this way is very effective and that the intestine regains its normal architecture after some time.
Treated patients (those who have remained off gluten and have a healthy intestine according to biopsy analysis) are sometimes re-exposed to gluten (gluten challenge) in the clinic to confirm diagnosis or to track drug efficacy in clinical trials.
Varied response to gluten challenge
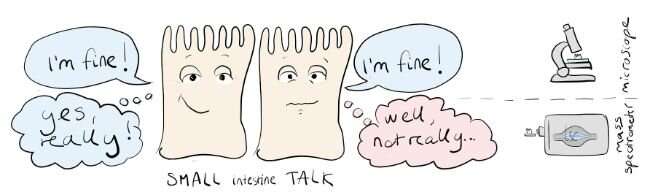
For reasons that are not completely understood, upon gluten challenge, some treated patients develop strong mucosal inflammation while others do not. This suggests that there are subtle differences between treated patients that are not easy to detect by visual inspection of intestinal biopsies alone, and that a more detailed picture of tissue status is needed to fully understand the connection between gluten exposure and disease severity.
That was the aim of the new study, led by Jorunn Stamnæs at the KG Jebsen Coeliac Disease Research Centre (JCoDiRC) at the University of Oslo.
Collaboration with NAPI
Jorunn collaborated with staff at the NAPI Proteomics Core Facility at Oslo University Hospital to perform mass spectrometry-based proteomics analysis of intestinal samples from a cohort of 19 well-treated celiac disease patients subjected to gluten challenge.
Although the 19 patients all were categorized as well treated prior to gluten challenge, they react very differently to the gluten—with strong mucosal changes in some patients and no observable changes in other patients.
The researchers used biopsies from all patients both before and after short-term gluten exposure, which allowed unbiased global analysis of the protein profiles associated with the different levels of inflammatory response.
Proteomics paints clearer picture
The proteomic approach revealed that patients with a strong inflammatory response had signs of ongoing ‘basal’ inflammation before re-exposure to gluten. This coincided with increased levels of gluten-specific T cells in the intestine, as well as a low-level presence of inflammatory proteins in the blood.
Although all patients in this cohort were considered well-treated by a standard gluten-free diet, gluten-related inflammation could still be ongoing at low level in the patients that responded strongly to gluten re-exposure. As these patients had a ‘head start’ they rapidly developed clear mucosal destruction.
Alternative approaches to categorize patients
These findings provide valuable new insights into celiac disease mechanisms, and raise the question as to whether a standard gluten-free diet is sufficient to fully ‘cure’ all celiac patients.
The research also suggests that, whilst manual inspection of intestinal biopsies is a valuable tool to broadly categorize disease status and response to gluten, alternative approaches such as proteomics could help to better define which patients still demonstrate low-level gluten-specific immune responses. A significant number of patients previously thought to be well-treated by a gluten-free diet may in fact require additional interventions to fully curb their gut inflammation.
Source: Read Full Article