Sudden smell and taste loss has become a well-known symptom of COVID-19. However, some people have also woken up to discover that their usual beloved coffee odor has been distorted and now smells like garbage or rotting meat, a condition known as parosmia. Others smell cigarette smoke, for example, when no odor source is present, a condition called phantosmia.
Now, investigators at the Monell Chemical Senses Center have teased out the differences between these two conditions and describe them in the peer-reviewed journal Chemical Senses. Knowing the distinct patterns of demographics, medical history, and quality-of-life issues associated with each condition may provide insight into the organization and function of the olfactory system, as well as help physicians better treat their patients.
“It’s clear from our results that these distortions in smell are distinct and common among those with smell impairment,” said lead author Robert Pellegrino, Ph.D., a Monell postdoctoral fellow. “Identifying patterns in these conditions is a first step to discovering their underlying biological cause.
“We hope this work will attract more research on the reason for these conditions, followed by intervention to help these patients.” For example, the team discovered that parosmia tends to occur three to six months after smell loss, so while this smell distortion has a huge effect on quality of life, it typically resolves faster than phantosmia or smell loss. “And that’s extremely useful for some patients to know,” he added. Despite the obvious differences between parosmia and phantosmia, most studies do not separate them in their analyses and have not gathered quantitative data, instead relying on narratives of anecdotal patient experiences.
Pellegrino suspected there might be important lessons to learn by studying what is unique about each condition. He designed a survey that produced quantitative data to describe each state, which allowed him to compare and make conclusions about the differences between the conditions. From this, they created a severity metric for research and clinical use, based on the combined frequency and duration of distortion episodes. “There are major differences in patients’ experiences with these distortions, with some more severe than others and the capacity to cause significant impact on their quality of life,” said Pellegrino. “For instance, these patients frequently report that they are continually reminded of their disorder, which may lead to such mental health conditions as depression.”
The team surveyed over 2,100 people with at least one olfactory disorder acquired during their lifetime. They found that odor distortions were common at 46 percent, with respondents reporting either parosmia at 19 percent, phantosmia at 11 percent, or both at 16 percent. They used an online questionnaire distributed globally in English, with the United Kingdom and the United States representing the largest proportion of respondents. Primary areas of recruitment were the website of the patient advocacy group AbScent and social media posts to AbScent’s Facebook and Twitter accounts. Survey data were collected between May 2019 and October 2020.
The distinctions between the disorders include:
- Age and gender: Parosmia patients were more likely to be female and younger than individuals who were phantosmic or had full (anosmic)/partial smell loss (hyposmic). In contrast, phantosmia was more prevalent in 41–50 years olds, and anosmia or hyposmia was more prominent in older individuals. There were no differences in gender between phantosmic vs. anosmic or hyposmic sufferers.
- Cause: Viral infection led to parosmia more often than other smell disorders, while traumatic impact to the head led to phantosmia more often than other disorders.
- Improvement timeline: Parosmic individuals were more likely to say their condition improved over time and recovery coincides with the timeline of physiological recovery. On the other hand, phantosmia was more stable, with no change in improvement across time.
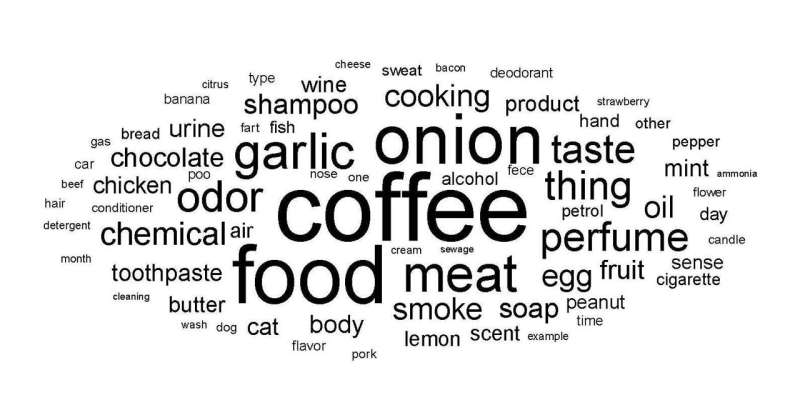
- Triggers: Most parosmic patients cited specific distorted sources of smell, while only a few phantosmic individuals could identify a source of their smell distortions. When describing the triggers of distorted smelling episodes, parosmic individuals cited odors, such as roasted coffee or garlic. In contrast, phantosmic sufferers noted locations, time, specific sensory input, stress, or memories.
The neurological mechanisms of parosmia and phantosmia are still debated among scientists. The Monell team’s work supports a parosmia hypothesis that a sensory neuron (located in the nose) tuned to one odor mistakenly signals the presence of a different odor. “This miswiring may create a flip in the odor perceived, with good odors smelling bad and bad odors smelling good,” said Pellegrino. Phantosmia, on the other hand, might happen if the brain is discharging sporadic signals, leading to odor hallucinations in an individual. Next steps to untangle the cause include confirming these ideas in animal models and translating findings back into treatments to help the patients who report a dramatic impact to their quality of life.
Source: Read Full Article