
While cancer patients and their doctors focus on eradicating their disease, there is often another life-threatening health issue developing throughout the course of treatment. Cancer therapies such as chemotherapy, radiation and immunotherapy can each cause unique and serious damage to the heart. As cancer treatments advance and more patients survive the disease, cardio-oncologists at National Jewish Health focus on cancer patients’ heart health to ensure they remain strong enough to endure treatment and to monitor their increased risk for cardiac events for years to come.
“I am with my patients throughout their entire cancer journey and well after remission. It’s my job to make sure each patient’s heart is as healthy as possible, so they can focus their mental and physical energy where it’s needed most, and that’s with battling cancer,” said Chris Fine, MD, a cardio-oncologist at National Jewish Health. “We monitor the heart closely, stratify patients’ risks for developing adverse effects and intervene early, before patients experience symptoms. The goal is to not only protect their heart health in the future, but also to avoid interruptions in cancer treatment over concerns that their heart isn’t strong enough.”
Cardiac toxicities can happen within the first few months of treatment or 20 years later. Each treatment comes with different concerns, but may include increased risk for heart attack, stroke and heart failure through atherosclerotic disease, valve disease and hardening of the arteries or heart wall.
Cardio-oncologists work closely with other cancer care providers to make informed decisions throughout their treatment and to provide seamless care that considers patients’ health as a whole, rather than cardiology and oncology separately. They see patients for routine imaging and testing through echocardiograms, EKGs and blood tests.
“Historically, cardio-oncology couldn’t even be a discipline because we were finding cancer too late and the prognosis for patients with cancer was quite poor. So, they never had the opportunity to develop cardiovascular toxicities,” Dr. Fine said. “As screenings and treatments have advanced and more patients are living longer, protecting their heart needs to be a part of the care. Cardio-oncologists are fully-equipped to understand the risks based on each patient’s unique situation and to merge their cardiac and cancer care to achieve the best outcomes possible.”
For Janet Schmidtlein-Sparling, Dr. Fine has not only been an important part of her cancer care team, but also part of the support system that helps her to keep fighting. Schmidtlein-Sparling was diagnosed with colorectal cancer in 2016, which has since metastasized to different parts of her body.
“The first time I met Dr. Fine I told him, ‘I’m not ready to give up yet,’ and he said, ‘Then I’m walking with you,'” Schmidtlein-Sparling said. “It’s very nice to know you have a doctor that’s going to be there to support you through cancer treatment, be aware of what the cancer and those treatments are doing to your body and help you to survive while going through it.”
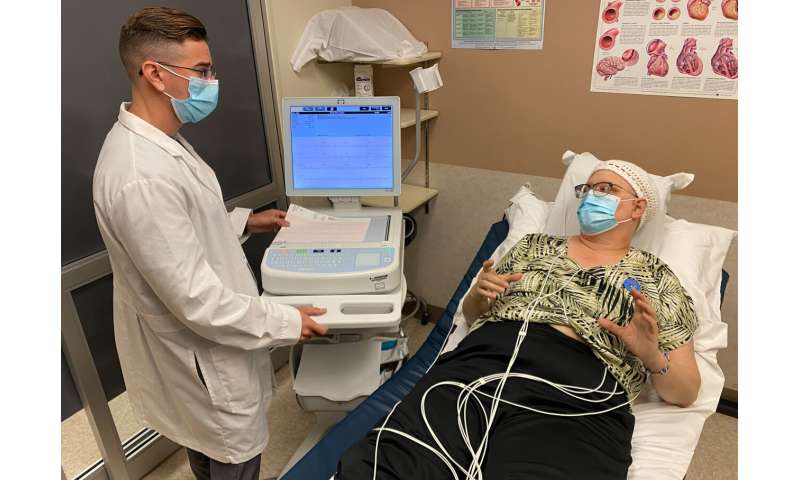
In addition to regular EKGs, Dr. Fine also asks Schmidtlein-Sparling to use an app on her phone to enter daily data for things like blood pressure, exercise, diet and blood oxygen levels. They review the data together to identify any subtle changes to her heart health.
“Prevention is key, and there are a lot of issues that we can see coming by just looking at the information at hand. We can identify changes over several weeks or months through data on a simple tracking app, and there are medications and interventions that we can implement early, at the first evidence of these heart-related toxicities,” Dr. Fine said. “And, although cancer patients often feel tired or have reduced appetite, it’s also important to have a medical professional who is encouraging them to remain active and to eat well, which can really go a long way for their heart and their overall health throughout treatment.”
Source: Read Full Article