New research from Baylor College of Medicine and Texas Children’s Cancer Center characterizes a new molecular type of high-risk pediatric liver cancer. The study, published in the Journal of Hepatology, showed that these tumors have better outcomes when patients were treated by transplantation, rather than by chemotherapy and surgery alone.
“Until recently, nearly all pediatric liver cancers were classified as either hepatoblastoma or hepatocellular carcinoma,” said Dr. Pavel Sumazin, associate professor of pediatrics at Baylor College of Medicine and Texas Children’s Cancer and Hematology Center and the first author of the study. “However, pediatric pathologists observed that some liver tumors have histological features that do not easily fit the hepatoblastoma or hepatocellular carcinoma models. These cancers are less likely to respond to chemotherapy, and patient outcomes are poor.”
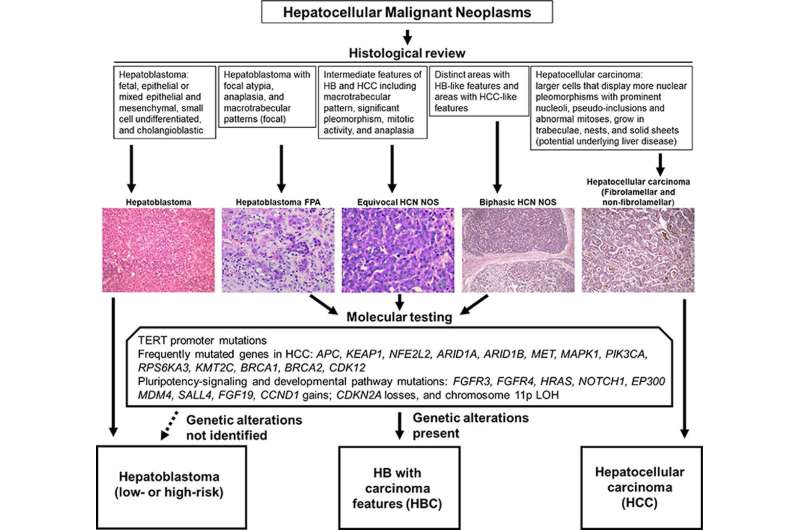
The researchers examined the molecular profiles of the tumors, including genetic alterations and gene expression profiles, and they found that these profiles do not fit into the hepatoblastoma (HB) or hepatocellular carcinoma (HCC) molecular categories. Instead, these tumors exhibited recurring molecular features that have been observed in both HBs and HCCs. They designated these tumors as hepatoblastomas with hepatocellular carcinoma features (HBCs).
The team also examined HBC treatments and outcomes and found that they tended to be more resistant to standard chemotherapy and have poor outcomes when not treated with more aggressive surgical approaches, including transplantation. Based on their findings, the team proposed a diagnostic algorithm to stratify HBCs and guide specialized treatment.
Source: Read Full Article