The first FDA-approved gene therapies are living drugs: immune cells taken from cancer patients engineered to target tumor cells. However, for many patients, these advanced therapies do not result in a long-lasting remission. Now, scientists at the New York Genome Center and New York University have developed a genetic screening platform to identify genes that can enhance immune cells to make them more persistent and increase their ability to eradicate tumor cells.
In the journal Nature, the researchers describe the discovery of synthetic gene programs that profoundly rewire a specific kind of immune cell called T cells, making them more effective at finding and fighting cancer cells. The research team, led by Neville Sanjana, Ph.D., Core Faculty Member at the New York Genome Center, Assistant Professor of Biology at New York University, and Assistant Professor of Neuroscience and Physiology at NYU Grossman School of Medicine, profiled the impact of nearly 12,000 different genes in multiple T cell subsets from human donors. The goal of this large-scale genetic screen was to identify precisely those genes that enable T cells to proliferate and to understand how those genes impact other aspects of immune cell function relevant to fighting cancer.
Previous efforts to engineer T cells have focused on the targeting of specific tumor types by careful selection of cancer or tissue-specific proteins (antigens). Since first developed more than 30 years ago, chimeric antigen receptor (CAR)-T cell therapy has proven highly effective in targeting blood cancer cells, resulting in multiple FDA-approved CAR-T therapies. CAR-T cells have antigen receptors on their surface that recognize specific proteins present on cancer cells to target and destroy them. Some patients are cancer free even a decade after their CAR-T cell therapy, as the T cells introduced years earlier are still doing their job. But one of the major challenges facing biomedical science is to understand why a large majority of cancer patients who receive CAR-T cells fail to achieve lasting remission.
Dr. Sanjana, senior author of the study, explained, “To date, genetic engineering of T cells has been focused on finding new antigens or new CARs. We took a radically different approach: Instead of changing the antibody, we thought why not try adding genes that transform T cells into more aggressive cancer fighters? These modifier genes worked very well in blood cancers, and we believe they will likely work for multiple antigens and in solid tumors.”
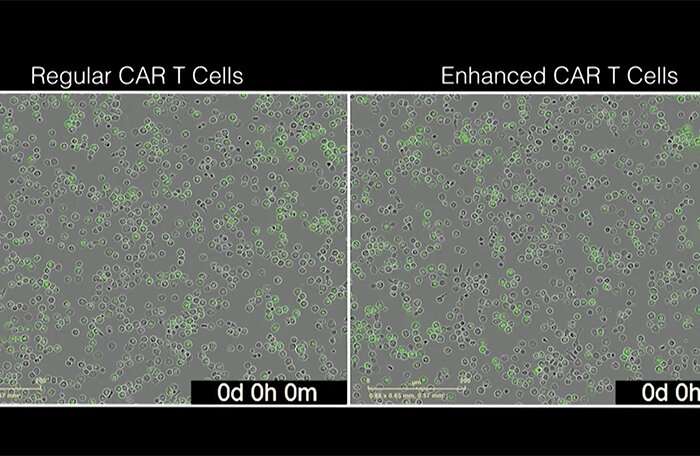
By combining modifier genes identified in the screen with existing CARs, the researchers were able to engineer T cells that were more effective at eliminating tumor cells. One particular modifier gene, lymphotoxin beta receptor (LTBR), acts like a molecular fountain of youth: With LTBR, T cells multiply, have a greater proportion of younger, more stem cell-like cells and resist becoming exhausted over time. Adding LTBR also caused T cells to secrete more cytokines, which are vital for the anti-tumor activity of T cells. Cytokines play an essential role in enabling T cells to better communicate with other immune cells in the body and launch coordinated attacks on the cancer. Interestingly, LTBR is not normally expressed in T cells, which highlights the power of the genome-scale screen to find genes that activate completely new cellular programs.
“Our goal was to take existing immunotherapies and make them better. We were astonished that LTBR so significantly potentiates CAR therapies. It is an important step forward towards the development of next-generation CAR-T cell therapy,” said the study’s first author Mateusz Legut, Ph.D., a postdoctoral fellow in the Sanjana Lab. The research team found that adding LTBR rewires the genome of T cell, triggering expression of many other genes that potentiate T cell function. The team was able to quickly understand the effects of LTBR and similar modifier genes by combining gene overexpression screens with single-cell genomics. The new method that they developed—OverCITE-seq—allowed the researchers to test the impact of different modifier genes on the cellular states of T cells, which includes the expression of every gene, the proteins decorating the cell surface, and the unique T cell receptors expressed by each cell (clonotype). OverCITE-seq gave the researchers a detailed picture of how each modifier gene boosts T cell activity and did so for all of the top-ranked genes in one single-cell experiment. For LTBR, this yielded an early clue that a large number of genes were changing, leading the researchers to further identify a well-studied modulator of gene expression called NF-kB driving many of these changes. This LTBR-driven profound reprogramming was also seen in so-called unconventional T cells such as γδ T cells, which are present at a lower abundance than conventional T cells but can target a more diverse set of tumors.

“The most exciting aspect is the demonstration that LTBR and other highly ranked genes improved the antigen-specific responses of chimeric antigen receptor T cells and γδ T cells. If validated in vitro and in clinical testing, this may have profound implication for future CAR-T cell therapies in both lymphoid malignancies and other cancers.” said study co-author Catherine Diefenbach, MD, an Associate Professor in the Department of Medicine at the Grossman NYU School of Medicine and the Director of the Clinical Lymphoma Program at NYU’s Perlmutter Cancer Center. The team also combined several top-ranked genetic modifiers with CARs similar to two existing FDA-approved therapies for blood cancers: tisagenlecleucel (Kymriah) and axicabtagene ciloleucel (Yescarta). Virtually all modifiers tested boosted CAR-T responses, including LTBR. Since T cells from cancer patients tend to be in poor condition compared to T cells from healthy donors, the researchers wanted to also test LTBR’s ability to rejuvenate cancer patient T cells. They added LTBR together with a CAR to dysfunctional T cells from patients diagnosed with diffuse large B cell lymphoma, a blood cancer, and found a similar boost in T cell function, suggesting that the technology could work as an optimized therapy in the clinic.
Andrew Sewell, Ph.D., an expert in T cells and immunotherapy from Cardiff University’s School of Medicine who was not involved in the study noted, “Gain-of-function screening in T cells has great potential to uncover how to make immunotherapies more successful—especially in solid cancers where current CAR T cell therapies do not work well.” The research team also showed that T cells enhanced with modifier genes were better able to eradicate not only leukemia but also pancreatic cancer cells. Those results are encouraging not only to develop a larger panel of enhanced CAR-T therapies for blood cancers, but for the key role they could play in targeting solid tumors, a field in which establishing efficient CAR-T immunotherapy has been more challenging.
Source: Read Full Article