For the first time, researchers at the University of Gothenburg have shown that metastases in patients with malignant melanoma gain access to the circulatory system not only through the outgrowth of new blood vessel branches, but also an alternative process in which one blood vessel divides into two parallel vessels by longitudinal splitting. The finding revisits an old research idea about how the growth of tumors can be inhibited by blocking formation of new blood vessels.
Like all other organs, tumors need access to the circulatory system to grow. Fifty years ago, a physician and researcher in the U.S., Judah Folkman, suggested that cancer cells trick the body into giving tumors access to the circulatory system by secreting molecules that stimulate the growth of new blood vessels.
Folkman then also suggested that tumors without access to blood vessels could never become larger than approximately one millimeter in diameter. This began many years of intensive work among cancer researchers, which in the 1990s resulted in identifying VEGF as the growth factor that signals adjacent blood vessels that they should create a new branch. It was hypothesized that blocking VEGF would stop growth of all solid cancer tumors.
But those hoping that this would become the great cure for all cancer with solid tumors were disappointed, because medications to block the growth factor had either no or limited effect in most cancers.
New way for blood vessels to spread
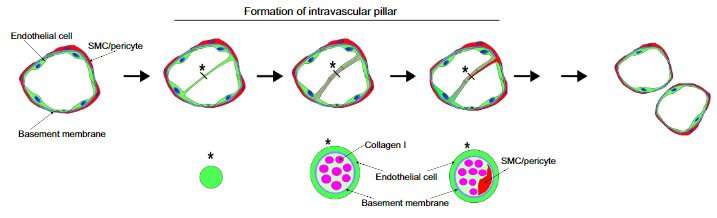
In the mid-1980s, in the shadow of intensive research on how new branches grow out of a blood vessel (known as sprouting angiogenesis), researchers in Switzerland showed that blood vessels can also divide longitudinally (intussusceptive angiogenesis). For nearly 200 years, researchers have known that blood vessels can grow with new branches, but intussusceptive angiogenesis is still relatively unknown.
In an extensive study, researchers at the University of Gothenburg have examined images of nearly 10,000 vessels in metastatic samples from patients with malignant melanoma. In a publication in American Journal of Pathology, they show that this form of angiogenesis occurs in metastases in malignant melanoma.
Time-consuming work
“This has taken a long time, where we carefully went through images from patients’ metastases to find the small structures that indicate the blood vessels are dividing,” says the work’s first author, Ankur Pandita. She is a doctoral student at the University of Gothenburg and a resident physician in oncology at Sahlgrenska University Hospital. “We have been looking for small intravascular pillars in the vessels, which occur just before the vessel divides. The pillars are extremely small, only one-twentieth the thickness of a hair.”
“The fact that tumors have an alternative way of accessing blood vessels may explain why VEGF inhibitors are inefficient in most tumors,” says Max Levin, associate professor at the University of Gothenburg and senior consultant in oncology at Sahlgrenska University Hospital. “Intussusceptive angiogenesis is an powerful way for blood vessels to spread in a tissue. In less than an hour, the blood vessel has formed the pillar that prepares it to divide.”
Possible medication
By combining epifluorescence and confocal microscopy, the team could visualize the pillars inside the vessels in the tumor samples. With RNA sequencing, researchers have begun to identify factors required for the division of blood vessels. A member of a group of enzymes known as matrix metalloproteinases (MMPs) seems to play an important role in dissolving blood vessel walls to permit the vessels to divide lengthwise.
“Our results suggests that intussusceptive angiogenesis contribute to the growth of daughter tumors in patients with metastatic malignant melanoma,” says Max Levin. “There are already pharmaceuticals today that inhibit MMP proteins, MMP inhibitors MMP inhibitors prevent the formation of pillars in experimental models, and the pharmaceuticals have the potential to be part of a treatment arsenal that can stop growth of metastases in patients with malignant melanoma.”
Source: Read Full Article