New study results suggest the national trend toward decreasing length of hospitalization after surgical procedures may come at the expense of an increasing proportion of complications occurring after patients leave the hospital. Findings from one of the few studies to explore the relationship between length of stay (LOS) and post-discharge complications for surgical patients were presented at the American College of Surgeons (ACS) virtual Clinical Congress 2021.
Hospitals have shortened inpatients’ hospital stays over the past two decades amid factors including an emphasis on outpatient treatment*, bed shortages, cost-cutting measures, and payers’ requirements. The new study found the median, or middle, crestor coupons LOS after an operation dropped by one-third, from three days in 2014 to two days in 2019.
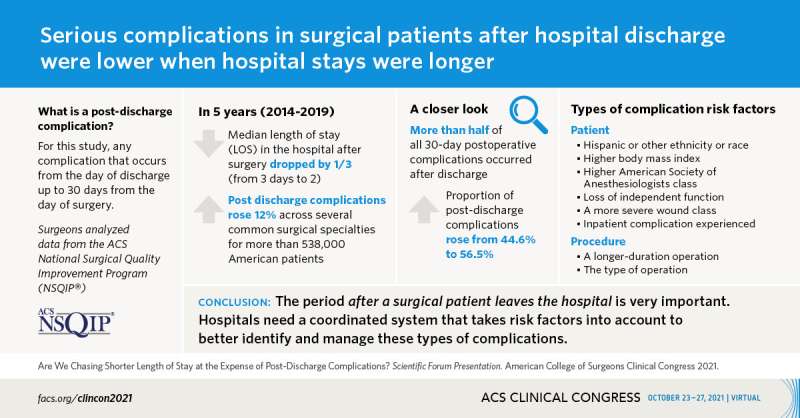
Although the researchers discovered that the overall rate of postoperative complications declined 1 percent over the five-year study, they found a 12 percent increase in post-discharge complications across several common surgical specialities for more than 538,000 American patients.
Multiple serious complications, including infections and heart problems, had significantly higher rates of occurrence after discharge in 2019, when the average hospital stay was shorter versus 2014, said study co-investigator Ruojia Debbie Li, MD, MS. Dr. Li is a research fellow at Northwestern University Feinberg School of Medicine, Chicago, where the study took place.
“There is a black hole that needs to be addressed between the time the patient gets discharged from the hospital to their first postoperative visit,” Dr. Li said. “Currently we are using a wait-and-see model where, as health care providers, we are waiting for surgical patients to approach us with any concerning signs and symptoms.”
Patients may not recognize complications
A shortcoming that emerges from this approach is that patients and their family caregivers often do not recognize early symptoms of complications, and then their problems may worsen, the study’s principal investigator, Ryan P. Merkow, MD, MS, FACS, assistant professor of surgery at Northwestern Medicine, said.
“I’ve found that many patients and their families are unprepared for the transition from hospital to home and for the task of self-care,” Dr. Merkow said. “The surgical team may not find out about a complication until the patient goes to the emergency room or comes for a clinic visit. If we had known earlier, we could have intervened and decreased the severity of the complication or even possibly have prevented it.”
Dr. Merkow said researchers typically count the rate of total complications within the first month after surgical procedures. This number combines complications occurring in the hospital and after discharge. Therefore, scant evidence exists on what effect a shorter hospital stay has on post-discharge complications, he said.
Post-discharge complications are on the rise
The research team studied the association between LOS and post-discharge complications using the ACS National Surgical Quality Improvement Program (NSQIP) database. NSQIP is the leading nationally validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care in hospitals and is aimed at reducing preventable postoperative complications.
Specifically, the researchers evaluated 2014 to 2019 data for patients who underwent any of 11 surgical procedures of the colon and rectum; esophagus; hepatopancreatobiliary system involving the liver, pancreas, gallbladder and bile ducts; or gynecologic or urologic systems.
Any adverse event occurring after the day of discharge but within 30 days of surgery was considered a post-discharge complication, Dr. Li explained. The researchers found the proportion of post-discharge complications rose from 44.6 percent in 2014 to 56.5 percent five years later.
Complications with significantly higher rates over time, according to Dr. Li, included surgical site infections and other infections such as pneumonia, urinary tract infection, or bloodstream infections known as sepsis. Other complications that increased as the LOS decreased were heart attack, cardiac arrest, or stroke and a serious blood clot called venous thromboembolism. Many of these complications are potentially preventable; for example, early recognition and management of a superficial wound infection could prevent consequences such as the surgical wound opening and/or sepsis.
Risk factors that were associated with a higher odds of post-discharge complications included:
- Patient factors: Hispanic or “other ethnicity/race”; higher body mass index; higher American Society of Anesthesiologists class (a surrogate for general health status used to predict operative risk); loss of independent function; higher wound class (a more severe wound); and experiencing an inpatient complication
- Procedure factors: a longer operation and the type of surgical procedure
Recommendations
“It is critical to not ignore this important period after the patient leaves the hospital,” Dr. Li said.
To lower the post-discharge complication rate, each hospital must have a coordinated system to better identify and manage these complications, Dr. Merkow stated. He recommended such a system include the following components:
- Education of patients and their family before the operation and before discharge, aimed at equipping them to recognize concerning signs and symptoms that they should discuss with their surgeon
- Easy communication between the patient and the surgical team
- Close monitoring that is more intensive for patients at elevated risk of complications
Source: Read Full Article