
A Northwestern University-led research team has developed a novel skin-mounted sticker that absorbs sweat and then changes color to provide an accurate, easy-to-read diagnosis of cystic fibrosis within minutes.
While measuring chloride levels in sweat to diagnose cystic fibrosis is standard, the soft, flexible, skin-like “sweat sticker” offers a stark contrast to current diagnostic technologies, which require a rigid, bulky, wrist-strapped device to collect sweat.
After developing the sweat sticker at Northwestern, the researchers validated it in clinical pilot studies involving cystic fibrosis patients and healthy volunteers at the Cystic Fibrosis Center at the Ann & Robert H. Lurie Children’s Hospital of Chicago. The sticker showed enhanced performance in collected sweat volume and equivalent accuracy to traditional platforms.
The research and study findings will be published on March 31 as the cover feature article in the journal Science Translational Medicine.
By softly adhering to the body, the millimeter-thick sticker makes direct but gentle contact with the skin without harsh adhesives. Not only does this make the sticker more comfortable and imperceptible to the wearer, this intimate coupling also enables the sticker to collect 33% more sweat than current clinical methods. The high collection rate ensures that one test will consistently collect a large enough sample to provide an accurate result.
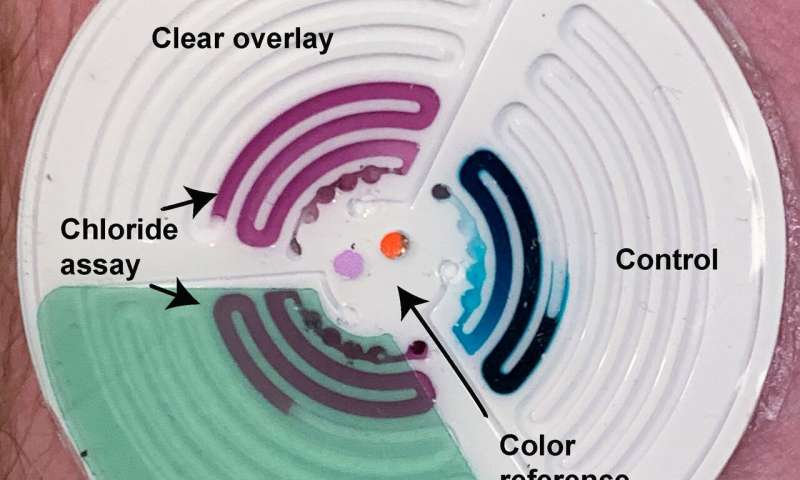
The sticker also has built-in colorimetric sensors that detect, measure and analyze chloride concentration in real time using a smartphone camera, bypassing the need for expensive laboratory equipment and excruciating wait times. This opens possibilities for testing outside of hospitals in the home setting, which could provide relief to parents in rural or low-resource areas without access to clinical centers with specialized diagnostic tools.
Biointegrated electronics pioneer John A. Rogers led the device development. Rogers is the Louis Simpson and Kimberly Querrey Professor of Materials Science and Engineering, Biomedical Engineering and Neurological Surgery in the McCormick School of Engineering and Feinberg School of Medicine and the director of the Querrey Simpson Institute for Bioelectronics (QSIB). Tyler Ray, who was a postdoctoral researcher in the Rogers lab at the time of the research, is the paper’s first author. He is now an assistant professor of mechanical engineering at the University of Hawai?i at Mānoa.
Challenges in sweat collection
The most-common life-shortening genetic disease, cystic fibrosis affects one in every 3,300 births in the United States and 70,000 people worldwide. Promising outcomes wholly depend upon early diagnosis. Because the disease attacks the digestive system, patients can become severely malnourished if they do not receive treatment soon after birth.
All newborns are screened for cystic fibrosis within the first few days of life through a heel prick. If that screen is abnormal, then pediatricians order a sweat test to confirm the diagnosis. During the sweat test, the baby must wear the hard, wrist-strapped device for up to 30 minutes. Sometimes smaller babies have trouble producing enough sweat for the test. Other times, the loose, ill-fitting sweat-collection device is unable to collect a large enough sample. In these instances, the baby must repeat the test at a later date, inducing anxiety and delaying treatment.
“Some parents bring their baby in for testing and are sent home without a confirmed result because the device was unable to collect enough sweat,” said study coauthor Dr. Susanna McColley, a cystic fibrosis expert and pediatric pulmonologist at Lurie Children’s Hospital and Northwestern Medicine. “They go home, without knowing if their baby has a serious disease or not, and their baby cannot yet start treatment. It can be agonizing.”
Unexpected collaboration
As former director of the clinical chemistry laboratory at Lurie Children’s, Shannon Haymond has witnessed this scenario too many times. Because of the poor fit and seal of the rigid collection devices on small infants’ arms, many families have experienced delayed results and diagnoses.
In fall 2016, the Rogers lab introduced a flexible sensor for the skin that could collect and analyze sweat in real time for health monitoring. After reading the paper, Haymond instantly saw the new device’s potential for cystic fibrosis.
“Many labs encountered problems caused by the current collection methods, making this a frequent focus of quality improvement efforts,” said Haymond, coauthor of the study and vice chair for computational biology and director of mass spectrometry at Lurie Children’s. “I thought the flexible skin sensors could simplify the process and improve collection results. And because the sweat stickers are disposable and designed for single use, they have an added advantage of preventing infection.”
Real-time results
By building sensing capabilities into the sticker, the Northwestern team offers potential for a speedier diagnosis. Users can simply snap a photo of the sweat-filled sticker and wirelessly transmit it to a clinic for quick analysis, alleviating diagnostic delays and allowing patients to start treatment as soon as possible.
“The device uses a network of microfluidic channels to collect sweat directly from the skin and route it to chambers to react with chemical reagents,” Ray said. “Those reagents cause a change in color that correlates to the chloride concentration level. By collecting and analyzing sweat at the point of collection, we can enable an earlier diagnosis. This is crucial for preventing severe complications and improving long-term patient outcomes.”
Routine monitoring from anywhere
Next, the team believes its sweat sticker could be used to routinely track cystic fibrosis patients’ long-term health and gauge how they respond to treatment. If the sticker detects a change in chloride levels, for example, that could inform a physician’s treatment plan.
“Because this device is untethered, we plan to use it beyond clinical environments,” said study coauthor Roozbeh Ghaffari, a research associate professor of biomedical engineering at Northwestern and director of translational research at QSIB. “In light of these new capabilities and further clinical validation, cystic fibrosis patients receiving treatment could someday use the sweat sticker at home to track their symptoms and hydration levels during daily living.”
Adding joy to the clinic
While running the clinical trials at Lurie Children’s, Dr. McColley noticed how much children loved the sweat stickers, especially compared to the traditional sweat tests.
Source: Read Full Article