Last year, the World Health Organization (WHO) announced an ambitious plan: to create a ‘cervical cancer-free future.” The potential reward is huge. If we succeed, cervical cancer will become the first cancer to be ‘eliminated’ on this scale.
But right now, around the world, someone dies every two minutes from cervical cancer, with lower resource countries more heavily impacted by the disease.
How do we get from figures like that to a world where cervical cancer is ‘no longer a public health problem’? And why cervical cancer in particular?
To help us unpick the strategy, we spoke to Professor Peter Sasieni, one of our researchers whose work is focused on cancer prevention, screening and early detection.
Sasieni has dedicated a large amount of his scientific career to understanding cervical cancer from a population perspective—understanding the disease not only in terms of its biology, generic medrol from india no prescription but also in terms of the big picture: who is at greatest risk of getting cervical cancer? And what can society do to reduce that risk?
Together, we talk through the commitment and innovation that will be needed to ensure this important milestone can become a reality.
Can cervical cancer be ‘eliminated as a public health problem’?
Let’s get down to it—what does it actually mean to eliminate cervical cancer as a public health problem?
There are some important nuances in language that Sasieni highlights here. It’s crucial to differentiate elimination as a public health problem as opposed to elimination (or eradication) of the disease.
Eradication of a disease in a country means there are no cases in that country. Smallpox, for example, has been eradicated worldwide. But elimination of a disease as a public health issue means to make it rare enough that it’s seen as something that affects a few individuals rather than a common disease affecting society as a whole.
“Having no cases left in the world is not WHO’s goal with cervical cancer,” he says. “But, if fewer than 4 women in every 100,000 worldwide each year were diagnosed with cervical cancer, that would be seen as eliminating it as a public health problem. To get there, we would need to prevent about 70% of cervical cancer around the world.”
So even if we do ‘eliminate’ cervical cancer, there will sadly still be people who develop it. But the goal is to make that number as small as possible.
To get there, WHO has devised the 90-70-90 targets around HPV vaccination, cervical screening, and effective treatment. These are milestones to be achieved by 2030 in order to make sure the world is on the right track towards ‘elimination.”
Why cervical cancer and why now?
“Why WHO have decided that now is the right time to implement a global strategy to eliminate cervical cancer as a public health problem is essentially because of the success of the HPV vaccine,” Sasieni explains.
Cervical cancer is unusual in that virtually all cases are caused by a virus called human papillomavirus (HPV), making it one of the most preventable cancer types.
HPV is an extremely common infection that infects the skin and cells lining the inside of the body. In most people, it doesn’t cause any problems at all.
There are over 100 types of the virus, and around 13 strains are known to be linked to cancer. “These strains can live in the cervix without you knowing for years and years, and then suddenly start causing a major health issue,” says Sasieni.
The link between HPV and cervical cancer was established in 1999, when a group of scientists, including Cancer Research UK scientist Professor Julian Peto, found that virtually all cervical cancer samples contained the virus.
Together, researchers proved that some HPV strains can cause cervical cancer. This was, and remains to this day, the risk factor that causes the largest proportion of a specific cancer worldwide. And it also gave scientists a new potential way to prevent the disease.
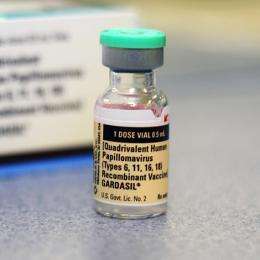
Years of international work, including a number of significant results from our scientists, resulted in the development of a number of vaccines that can prevent HPV infection. And after many promising signs, in 2020 the world got the first definitive evidence that vaccination could also reduce cervical cancer risk.
But vaccination is only part of the equation, Sasieni explains. “Relying only on vaccination means you’re looking at elimination in only people who have received the vaccine before exposure to HPV infection. So it’s important to have a combined strategy because otherwise you would only remove the disease amongst those people, which at the moment doesn’t include people over about 30, because of when vaccination started.”
So as well as the current vaccination program, the strategy outlines how to effectively implement cervical screening across the world.
Screening and vaccination in the UK
- In 2008, the UK implemented an HPV immunization program for adolescent girls.
- The HPV vaccine offered by health services in the UK protects against the 2 main types of HPV that together cause around 7 in 10 cervical cancer cases in the UK.
- This is now offered to all children aged 11 to 13 years old and is available on request to girls up to the age of 25.
- The UK currently has a national cervical screening program, which tests for HPV.
- The screening program invites women from age 25 to 64 for cervical screening, and cervical screening is also for trans men and non-binary people within this age range who have a cervix.
While screening and vaccination mean that elimination as a public health problem is a possibility, it has been projected that without further intervention, there would be 44.4 million cervical cancer cases diagnosed globally over the next 50 years.
And the burden of this disease falls heavily on women who live in the world’s poorest countries. As echoed by WHO, “few diseases reflect global inequities as much as cancer of the cervix”.
Elimination means elimination for all
Right now, the burden of cervical cancer falls predominantly on women in lower-resource countries, which account for 84% of cases and 90% of deaths from cervical cancer.
“It’s still a majorly important cancer, globally, affecting women relatively young. And with very high mortality rates in many countries,” says Sasieni. As WHO highlights, many of the women affected by cervical cancer have young children, impacting the entire family.
And for women with HIV, the chance of developing cervical cancer is 6 times higher than women who don’t have the virus.
Between 2006 – when the first HPV vaccine was approved – and 2014, more than 59 million girls worldwide received at least a single dose of the HPV vaccine. But when talking about the success of HPV vaccination, it’s important to note that only 15% of girls globally have been fully vaccinated.
Although the means for eliminating cervical cancer exist, they have not yet been widely actualised in parts of the world where the disease burden is greatest.
Now is the time to use the goal of elimination to motivate changes on the ground.
Overcoming barriers to vaccination
Sasieni highlights that both vaccination and screening programs vary on an international level. And both are extremely hard to implement and require a strong healthcare infrastructure.
WHO notes that high vaccine prices and recent supply challenges, in combination with issues of acceptance amongst the public, have made it difficult for many countries to introduce HPV vaccination or maintain existing programs.
As of 2020, fewer than 25% of low-income countries and fewer than 30% of lower-middle-income countries had introduced the HPV vaccine into their national immunization programs. This contrasts with more than 85% of high-income countries who have done so.
The first HPV vaccine approved for use was developed with the intention that every girl would receive 3 doses over a number of months. “The vaccine had to be kept in the fridge, you couldn’t freeze it, and you couldn’t let it get to room temperature. So that created a lot of logistical issues for trying to do it globally.”
But as well as storage, price was a huge challenge in a number of healthcare settings. “I think when the vaccines came out, it cost about $100 per dose. So $300 just to vaccinate one woman, making it near impossible for some places to afford.”
But things could be changing, as scientists look to reduce the number of doses.
“It’s now accepted that actually, 2 doses of the vaccine, instead of 3 is sufficient,” says Sasieni. This is reflected in WHO’s current guidelines, which recommend that girls aged 9 to 14 receive 2 doses of vaccine to be fully protected.
“But there’s increasing evidence that even one dose is really effective. And I would say that the evidence that one dose is more than half as good as 2 doses is extremely strong.”
It’s a theory we’re putting to the test. Together, with the Bill and Melinda Gates Foundation and the National Cancer Institute, we’re co-funding the PRIMAVERA trial. Based in Costa Rica, the trial is testing the potential of a single dose vaccine in preventing HPV infection and ultimately, cervical and other HPV-related cancers.
Although the study won’t be completed until 2023, if the results find that a single dose can trigger the same immune response against HPV, it could have a big impact on global vaccination efforts. To put it simply, countries would be able to double the number of girls vaccinated with the stocks available.
Sasieni weighs up the options. In his mind, the answer is clear. “If you said, well, I’ve got a million doses for this particular part of the world, should I try to vaccinate half a million women with 2 doses each, or a million women with 1 dose? I think if you are limited in your resource, then it’s pretty clear that that 1 dose for a million women is maximizing the benefit of that resource.”
Reducing cost is a big step in the right direction, but it’s not the only step needed.
Another important step is recognizing cultural barriers that might exist towards getting vaccinated, “I think it’s essential to understand cultural issues around vaccination, and people’s attitudes to vaccines.
“For HPV vaccination, there are additional concerns related to the fact that the virus is sexually transmitted. Some communities fear that the HPV vaccine might encourage promiscuity for example, because if someone’s been vaccinated against it, they might no longer worry about getting a sexually transmitted infection, or they might view having the vaccine as a ‘green light’ to become sexually active at an earlier age” says Sasieni.
“There’s no scientific basis for thinking that people change their behavior after getting vaccinated, but making it clear that this is a vaccine against cancer, is really important.”
And as Sasieni explains, vaccination alone is not the answer.
National screening programs
“Lots of my research has been linked to cervical screening,” says Sasieni.
Like HPV vaccination, “screening is very difficult to do well, and you need a pretty good health infrastructure. You need something that enables you to identify everyone in the population. Because otherwise, the people that will get screened will be those who are better off. So the first hurdle is you need to be able to invite everybody to do the screening.”
Cervical screening (previously known as a ‘smear test’) involves collecting samples of cells from the cervix using a small, soft brush, and then analyzing those cells in the laboratory.
In England, Scotland and Wales, the lab will first check if the sample has high risk HPV. High risk HPV can cause cell changes in the cervix, which over time can develop into cancer. If a sample has high risk HPV, the laboratory will examine the sample under a microscope to look for cell changes, and if cell changes are found, the person will be invited for a follow up test called a colposcopy.
But trying to replicate this in countries around the world may not be the best approach. With this process, transporting samples to the lab can throw up logistical problems that are hard to overcome. “If you’re in countries where it can get up to 40 or 50 degrees Celsius, putting samples in the post can cause problems where we can’t rely on the results of the test when the sample’s been at that sort of temperature for a number of hours.
“This type of molecular test is also difficult to organize in countries without a good health care infrastructure, and the biggest problem then is getting the test results to the women and ensuring that treatment is available.”
Sasieni mentions other ways of studying the cells, that can remove the difficult process of having to analyze them under a microscope in the lab. “I think, and possibly again with COVID-19, people will see that actually, there are a number of ways you can test for DNA,” he says.
“There may be new technologies that are allow rapid point of care testing, so that you could start having screening programs go into rural villages or crowded urban areas and get screening results back in an hour.”
In the last few years, scientists have developed HPV tests based on LAMP technology – a technique also used for rapid COVID-19 testing, which allows for the quick amplification and testing of DNA.
But the options don’t end there. “There are other HPV tests which can be done using a portable machine no bigger than a home printer,” Sasieni adds. “As well as several companies that are developing devices like mobile phones that take photographs or videos of the cervix and analyze them in real-time using artificial intelligence.”
Barriers and inequalities in screening
Getting the logistics right is the first hurdle, but it’s not the only one.
“Within countries there are almost certainly inequalities in terms of groups who are deprived because of language and ethnicity and access to healthcare communications. In many cultures, in families who have immigrated, women are less likely to know the language than men.
“Or, for example, if screening or intimate examination is done by a man, that would not be acceptable in some cultures.”
WHO’s strategy has outlined that strong communication strategies for effective advocacy can overcome the many challenges that might limit access to cervical cancer prevention and care, but that this content must be culturally relevant and context-specific.
This same sentiment is echoed by Sasieni, “you can’t just say one size fits all for how you should implement this strategy worldwide. Because there are a whole variety of things that need to be considered, from healthcare priorities, to infrastructure, to international trade.”
Another point that Sasieni draws attention to is the need for a national screening program to establish who they’ll invite for screening.
“One of the things that I’ve been trying to do with WHO is to get across this idea that there needs to be a catch up for screening, that we shouldn’t just write off everyone born before 1975, or maybe even 1980.”
But despite Sasieni’s efforts, there’s talk about not offering any screen to anyone over 45. “By the time a screening program is put into place, that could mean that anyone born before 1980 won’t benefit from WHO’s efforts to eliminate cervical cancer. And that would be tragic.”
Collaboration on a global scale
We’ve barely scratched the surface on all the factors that need to be considered when implementing this global strategy. But it’s clear that achieving cervical cancer elimination will not be possible without collaboration.
The WHO details the role of civil society, women’s groups, non-governmental organizations and a wide range of local networks being fundamental to the successful uptake of services at the community level.
Our international cancer prevention program is working with these organizations to advocate for greater HPV vaccine demand and acceptance around the world.
On an international scale, Sasieni highlights that there’s a lot that can be shared.
“Well, the UK has been really very involved in HPV vaccine research, and probably even more so, cervical screening research, HPV testing, and looking at biomarkers for triage,” says Sasieni.
Source: Read Full Article