Mutations from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have created multiple variants. Some variants, such as those found in South Africa and Brazil, have caused concern for their potential to evade the immune response. While vaccination efforts are underway, the world is racing against the viruses’ ability to evolve under selective pressure.
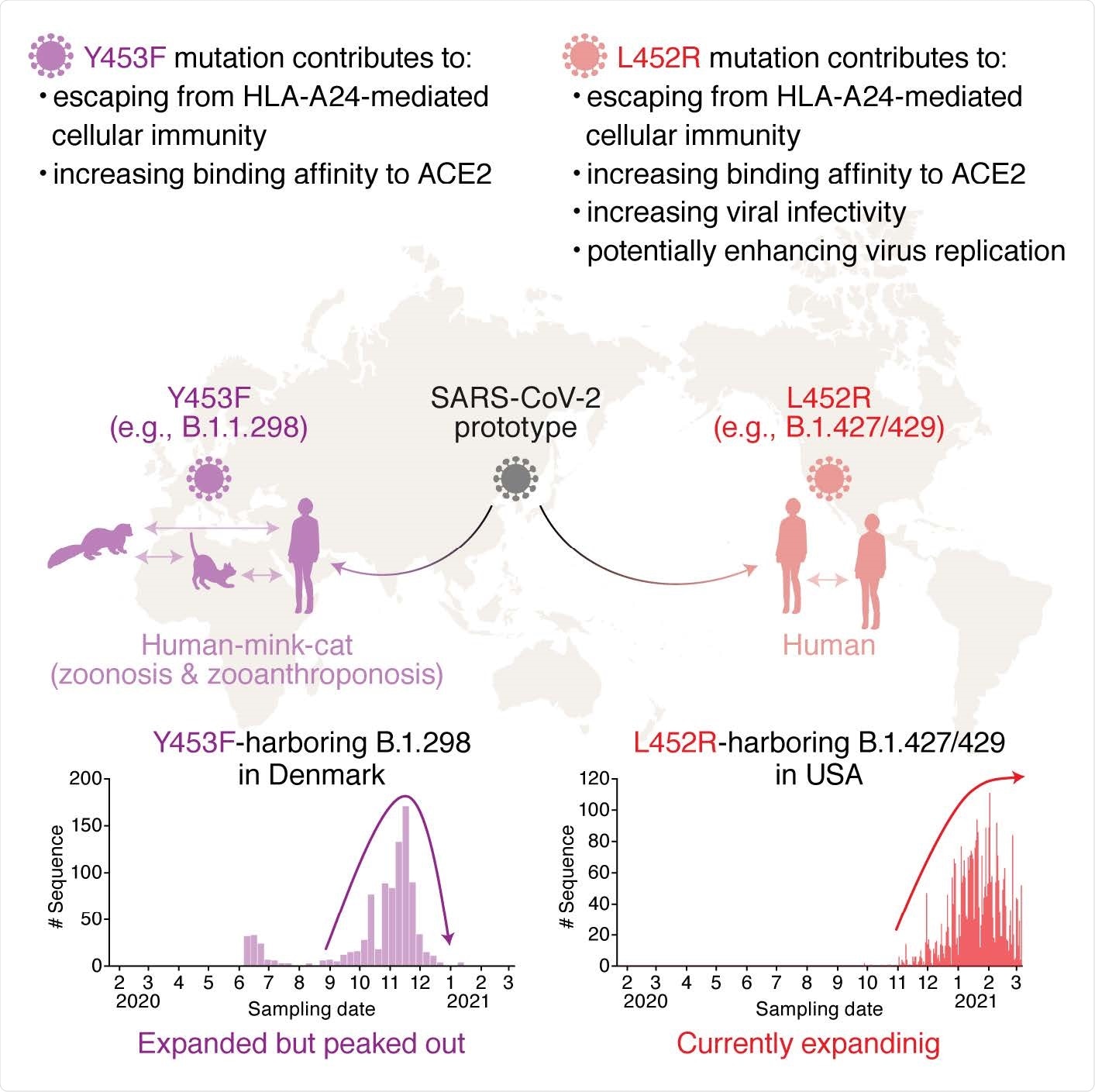
The B.1.427/429 variant first identified in California is a prime example of SARS-CoV-2’s efforts to prolong its survival by combining mutated variants to form a more durable product. A new study published in bioRxiv* suggests the magnitude of the threat SARS-CoV-2 mutations present to public health. Their results found the L452R mutation in B.1427/429 and Y453F mutation in the B.1.298 variant evade human leukocyte antigen (HLA)-restricted cellular immunity and increase binding affinity to viral receptor ACE2.
Immune evasion from spike protein mutations on the NF9 region
The researchers collected peripheral blood mononuclear cells from nine convalescent samples with prior exposure to COVID-19 to investigate how the SARS-CoV-2 mutations could cause resistance to antigen recognition through HLA-restricted cellular immunity. They focused their attention on 9-mer peptide in the RBM called NYNYLYRLF (NF9) because of prior research suggesting it is a potential epitope identified by the immune system.
They found CD8+ T cells with upregulated activation markers CD25 and CD137 in response to NF9. The presence of NF9 also significantly increased CD25+ CD137+ cells. Based on the results, the research team suggests the NF9 peptide is an immunodominant HLA*24:02-restricted epitope identified by CD8+ T cells. NF9 stimulation also increased cytokine production produced from CD8+ T cells such as IFN-γ, TNF-α and IL-2.
The team next looked at how variants in the area, specifically residues 448-456 in the spike protein, affects antigen recognition. They collected 750,243 viral genome sequences from the GISAID public database and found the L452R substitution to be the most frequent mutation — being present in 5,677 sequences. The Y453F substitution was present in 1, allied photo grand rapids 380 sequences. The team noted both mutations are present in the B.1.427/429 and B.1.1.298 lineages.
Using simulations of SARS-CoV-2 spike protein with NF9 derivatives having either the L452R or Y453F mutation, the team found the IFN-γ expression levels lower when the Y453F mutation was present in the NF9 region. With L452R, there was no expression of IFN-γ.
“Altogether, these results suggest that the NF9 peptide, which is derived from the RBM of SARS-CoV-2 S protein, is an immunodominant epitope of HLA-A24, and two naturally occurring mutants, L452R and Y453F, evade the HLA-A24-restricted cellular immunity.”
When analyzing binding affinity, they found the N501Y, Y453F, and the L452R mutations increased binding to human ACE2. They also observed the L452R mutation increased surface expression while the other two mutations did not. The results strongly suggest the L452R also helps with protein stability.
The team looked at viral infectivity in the presence of spike protein mutations. The N501Y mutation barely affected infectiousness, but the researchers did note the L452R mutations significantly increased infectivity compared to the SARS-CoV-2 spike protein without mutations. The Y453F mutation had lower viral infectivity than the parent spike protein.
While the L452R mutation is not directly on the binding interface, further analysis showed the substitution increases SARS-CoV-2 infectiousness by increasing electrostatic interactions with ACE2.
The increased viral infectivity from the L452R mutation also translated to increased viral replication compared to SARS-CoV-2 without mutations.
Altogether, the researchers found the L452R mutation and Y453F mutation in B.1.298 on the receptor-binding domain of SARS-CoV-2 can escape HLA-24-restricted cellular immunity. The mutations also reinforced the affinity to ACE2. The L452R mutation also increased protein stability, viral infection into human host cells and promoted viral replication in the body.
Mutation-harboring variants spread across the world
The evasion of cellular immunity could influence how future viral variants evolve, suggesting a further threat to the coronavirus pandemic.
The first L452R mutation was first detected in the B.1.39 lineage in Denmark in March 2020 — although it did not spread. On the other hand, L452R-harboring variants were also found in California in September 2020, spreading across the state. The researchers note the L452R mutation is increasingly expanding in the United States and is a predominant lineage in the country.
The Y453F mutation was first found in the B.1.1.298 lineage, which was first sequenced in Denmark in April 2020. The lineage peaked in Denmark from October to November 2020 before declining, with the last sequence containing the Y453F mutation found in Denmark on January 18, 2021.
Important Notice
*bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.
- Motozono C, et al. An emerging SARS-CoV-2 mutant evading cellular immunity and increasing viral infectivity. bioRxiv, 2021. doi: https://doi.org/10.1101/2021.04.02.438288, https://www.biorxiv.org/content/10.1101/2021.04.02.438288v1
Posted in: Medical Research News | Disease/Infection News
Tags: ACE2, Antigen, binding affinity, Blood, Coronavirus, Coronavirus Disease COVID-19, Cytokine, Genome, Human Leukocyte Antigen, Immune Response, Immune System, Leukocyte, Mutation, Pandemic, Protein, Protein Stability, Public Health, Receptor, Research, Respiratory, SARS, SARS-CoV-2, Severe Acute Respiratory, Severe Acute Respiratory Syndrome, Spike Protein, Syndrome

Written by
Jocelyn Solis-Moreira
Jocelyn Solis-Moreira graduated with a Bachelor's in Integrative Neuroscience, where she then pursued graduate research looking at the long-term effects of adolescent binge drinking on the brain's neurochemistry in adulthood.
Source: Read Full Article